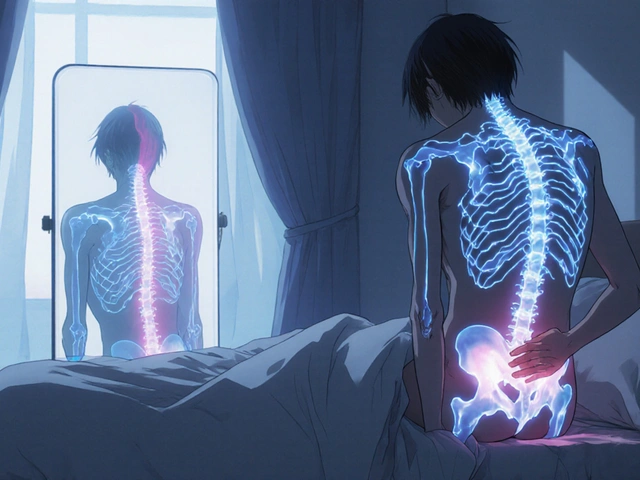
When you take cyclosporine, you're not just managing your immune system-you're navigating a minefield of hidden drug interactions. This powerful immunosuppressant, used after organ transplants and for severe autoimmune conditions, doesn't just sit quietly in your body. It actively interferes with how your liver and gut break down other medications. At the heart of this problem is the CYP3A4 enzyme-a key player in metabolizing nearly 60% of all prescription drugs. Cyclosporine doesn't just get broken down by CYP3A4; it shuts it down. And that can turn a safe dose of another drug into a dangerous overdose.
Why CYP3A4 Matters More Than You Think
CYP3A4 isn't just another enzyme. It's the workhorse of your body's drug-processing system. Found in your liver and intestines, it's responsible for breaking down everything from statins to antibiotics, painkillers, and even some cancer drugs. When CYP3A4 is working normally, it keeps drug levels in your blood balanced. But when something like cyclosporine steps in and blocks it, those drugs don't get cleared out. They build up. And because cyclosporine has a narrow therapeutic window-meaning the difference between an effective dose and a toxic one is small-any disruption can lead to serious harm.
Imagine you're on cyclosporine after a kidney transplant and your doctor prescribes a common antibiotic like clarithromycin to treat a sinus infection. Clarithromycin is a strong CYP3A4 inhibitor. When you take both, cyclosporine levels can spike by 2 to 3 times. That might sound like a small change, but in transplant patients, even a 20% increase in cyclosporine concentration can cause kidney damage. One study found that within 72 hours of starting clarithromycin, some patients saw their creatinine levels jump 40-60%, signaling sudden kidney stress. This isn't theoretical-it happens in real clinics every week.
Cyclosporine Isn't Just a Substrate-It's an Inhibitor
Many people assume that if a drug is metabolized by CYP3A4, it's just a passive passenger. But cyclosporine is different. It's both a substrate (something the enzyme breaks down) and a potent inhibitor (something that blocks the enzyme). This dual role makes it uniquely dangerous. Other immunosuppressants like tacrolimus are mostly substrates-they're affected by other drugs but don't usually interfere with them. Cyclosporine? It actively messes with the system.
Studies show cyclosporine doesn't just compete with other drugs for space on the enzyme (competitive inhibition). It also binds to CYP3A4 in a way that permanently damages it over time (mechanism-based inhibition). This means even after you stop taking the interfering drug, the enzyme doesn't bounce back immediately. It takes days for your body to make new CYP3A4. So if you're on cyclosporine and start a new medication, the interaction isn't just immediate-it lingers.
And it doesn't stop at CYP3A4. Cyclosporine also blocks P-glycoprotein, a transporter that pumps drugs out of cells. This dual action-slowing metabolism and trapping drugs inside cells-means interactions are more severe and harder to predict than with most other drugs.
What Medications Are Most at Risk?
If you're taking cyclosporine, you need to know which drugs could turn dangerous when combined with it. Here are the biggest red flags:
- Sirolimus and everolimus: These are other immunosuppressants often used alongside cyclosporine. When taken together, cyclosporine can boost sirolimus levels by over 200%. That's why doctors typically cut sirolimus doses by 70% when starting both drugs.
- Statins: Atorvastatin, simvastatin, and lovastatin are all broken down by CYP3A4. With cyclosporine blocking the enzyme, these can build up to toxic levels, causing severe muscle damage (rhabdomyolysis). Rosuvastatin and pravastatin are safer alternatives because they don't rely on CYP3A4.
- Calcium channel blockers: Diltiazem, verapamil, and nimodipine can raise cyclosporine levels by 30-50%. In return, cyclosporine can make these drugs too strong, leading to low blood pressure or heart rhythm issues.
- Antifungals: Fluconazole, itraconazole, and ketoconazole are strong CYP3A4 inhibitors. Using them with cyclosporine can trigger kidney failure or neurotoxicity.
- Some antidepressants and antipsychotics: Sertraline, fluoxetine, and risperidone can accumulate to dangerous levels when CYP3A4 is blocked.
Even over-the-counter supplements like St. John’s wort can be risky. It's an inducer-it speeds up CYP3A4-which can make cyclosporine levels crash and trigger organ rejection. One patient in a 2021 study stopped taking cyclosporine after starting St. John’s wort for anxiety and had a kidney transplant rejection within two weeks.

How Doctors Manage These Interactions
Managing cyclosporine interactions isn't guesswork. It's a science. Transplant centers follow strict protocols:
- Screen every medication: Pharmacists review every pill, patch, or injection a patient is taking-even vitamins and herbal products.
- Use therapeutic drug monitoring: Blood tests check cyclosporine levels regularly. After starting a new drug, levels are checked daily for the first week.
- Dose adjustments are standard: If you start a moderate CYP3A4 inhibitor like diltiazem, your cyclosporine dose is usually lowered by 25-50%. For strong inhibitors like clarithromycin, the reduction can be 50-75%.
- Switch to safer alternatives: If possible, doctors avoid CYP3A4 inhibitors altogether. For example, they might choose azithromycin instead of clarithromycin, or cefdinir instead of a statin that interacts.
One 2022 study across 12 transplant centers showed that using electronic alerts in hospital systems, paired with pharmacist reviews, cut cyclosporine-related hospitalizations by 45%. That’s not just a number-it’s lives saved.
Genetics Play a Bigger Role Than You Realize
Not everyone processes cyclosporine the same way. Your genes matter. Some people have natural variations in the CYP3A4 enzyme that make it less active. Others have more of CYP3A5, another enzyme that can help break down cyclosporine. People with certain genetic types (like CYP3A4*22) can have up to 40% slower metabolism of cyclosporine. That means they need lower doses just to stay in the safe range.
Researchers at Wenzhou Medical University found that combining genetic testing with drug interaction data could predict cyclosporine levels with 85-90% accuracy. That’s not science fiction-it’s already being used in some European transplant centers. The European Society of Organ Transplantation now recommends CYP3A4 genotyping for new patients to guide initial dosing.

What You Can Do to Stay Safe
If you're on cyclosporine, here’s what you need to do:
- Never start a new medication without telling your transplant team. That includes OTC drugs, supplements, and herbal remedies.
- Keep a complete, up-to-date list of everything you take. Include doses and how often you take them. Bring this list to every appointment.
- Ask your pharmacist: "Does this interact with cyclosporine?" They have access to tools that flag interactions in real time.
- Know the signs of toxicity: Unexplained nausea, vomiting, tremors, swelling in your legs, or sudden changes in urine output could mean your cyclosporine level is too high.
- Don’t skip blood tests. These aren’t just routine-they’re life-saving.
The Bigger Picture: Why Cyclosporine Still Matters
You might wonder why we still use cyclosporine when newer drugs like tacrolimus exist. The answer? It still saves lives. While tacrolimus is now the first choice for most adult transplants, cyclosporine remains vital for children, patients with certain autoimmune diseases like psoriasis or nephrotic syndrome, and those who can't tolerate other drugs. The global market for cyclosporine is still growing-projected to hit $2.4 billion by 2030.
Its future isn't about being the strongest immunosuppressant. It's about being used safely. With better monitoring, genetic testing, and smarter prescribing, cyclosporine can keep working for decades to come. But only if we stop treating it like just another pill. It's a powerful tool-and like any tool, it demands respect.
Can I take ibuprofen with cyclosporine?
Short-term use of ibuprofen at low doses is usually okay, but it’s not risk-free. Both cyclosporine and ibuprofen can stress your kidneys. Taking them together increases the chance of kidney damage, especially if you’re dehydrated or already have reduced kidney function. Always check with your doctor before using any NSAID, even over-the-counter ones. Acetaminophen (Tylenol) is a safer option for pain relief.
How long does it take for cyclosporine interactions to show up?
Some interactions happen within hours-especially with strong inhibitors like clarithromycin or ketoconazole. Cyclosporine levels can peak in 24-72 hours after starting the interacting drug. But because cyclosporine also causes time-dependent inhibition, the full effect can take days to build. That’s why doctors monitor blood levels daily when starting a new medication.
Is cyclosporine the only immunosuppressant with this problem?
No, but it’s one of the worst. Tacrolimus is mainly a substrate-it’s affected by other drugs but doesn’t usually block CYP3A4. Sirolimus and everolimus are also substrates. Cyclosporine is unique because it’s both a substrate and a strong inhibitor. This dual role makes it the most likely drug to cause dangerous interactions in transplant patients.
Can grapefruit juice affect cyclosporine?
Yes, and it’s a big deal. Grapefruit juice is a strong CYP3A4 inhibitor. Even one glass can raise cyclosporine levels by 30-50%. If you’re on cyclosporine, avoid grapefruit, Seville oranges, pomelos, and their juices entirely. Don’t assume "a little" is safe-there’s no safe amount.
What should I do if I miss a cyclosporine dose?
Don’t double up. If you miss a dose by less than 6 hours, take it as soon as you remember. If it’s been more than 6 hours, skip the missed dose and take your next one at the regular time. Missing doses can cause cyclosporine levels to drop, increasing rejection risk. But doubling up can cause toxicity. Always call your transplant team if you’re unsure.
Final Thought: Knowledge Is Your Shield
Cyclosporine isn’t a drug you take and forget. It demands attention. Every new prescription, every supplement, every cold medicine-it all matters. The good news? With careful monitoring, clear communication, and smart choices, you can use cyclosporine safely for years. The science is clear. The tools exist. What matters now is that you’re informed-and that you speak up when something doesn’t feel right.





Jennifer Shannon
Wow, this post is like a masterclass in how our bodies are these delicate, overworked factories with zero union representation. CYP3A4 is basically the tired barista who’s juggling 17 drinks at once, and cyclosporine? It’s the guy who walks in, slams his hand on the counter, and says, ‘I’m taking over the espresso machine-and don’t you dare make another latte.’ And then, just to be dramatic, it breaks the machine slowly, over days. I mean, we’re talking about a drug that doesn’t just interact-it *dominates*. It’s less like a medication and more like a silent film villain in a lab coat. And yet, people still take it? Because, as the article says, it saves lives. That’s the tragic beauty of modern medicine-we’re constantly trading one kind of danger for another. And somehow, we’re still alive. I’m just glad I’m not the one trying to calculate the math on my kitchen table at 2 a.m.
Suzan Wanjiru
Statin interactions are the silent killer here. People think they’re just taking a cholesterol pill but don’t realize they’re risking rhabdo. Always check with your pharmacist. Rosuvastatin or pravastatin are your friends. And grapefruit juice? Just say no. Full stop.
Kezia Katherine Lewis
The dual pharmacokinetic profile of cyclosporine-as both substrate and mechanism-based inhibitor of CYP3A4-creates a uniquely complex drug interaction landscape. This is compounded by its concomitant inhibition of P-glycoprotein, which exacerbates intracellular accumulation of co-administered agents. Consequently, therapeutic drug monitoring remains indispensable, particularly during initiation or titration of concomitant medications with known CYP3A4 modulatory effects. Genetic polymorphisms in CYP3A4/5 further necessitate individualized dosing strategies, as evidenced by emerging pharmacogenomic protocols in European transplant centers.
Henrik Stacke
Oh my goodness, this is one of the most terrifyingly beautiful pieces of clinical pharmacology I’ve read in years. I mean, imagine your liver is a busy airport, and every drug is a plane. Cyclosporine? It doesn’t just land-it shuts down the entire control tower, steals the runway keys, and then *keeps* the keys for days after it’s gone. And we wonder why people end up in the ICU? This isn’t just a warning-it’s a love letter to pharmacists everywhere. Thank you for being the unsung heroes who catch these disasters before they happen. I’m sending virtual tea and cookies to every hospital pharmacy in the world right now.
Kane Ren
Knowledge really is power here. I’ve been on cyclosporine for 8 years now, and I used to skip blood tests when I felt fine. Big mistake. I got sick once because I took a random painkiller. Now I carry my med list everywhere. It’s a hassle, but I’m alive. So don’t be lazy. Talk to your team. You’ve got this.
Charmaine Barcelon
Ugh, why do people even take this drug anymore? It’s a nightmare. I’ve seen so many patients crash because they took ibuprofen or drank grapefruit juice. It’s not rocket science. Just don’t do it. If you can’t follow the rules, maybe you shouldn’t be on it. This isn’t a hobby-it’s life or death. And no, ‘I thought it was fine’ doesn’t cut it.
Pramod Kumar
Man, this hits different. I remember my cousin in Delhi-he got a kidney transplant, started cyclosporine, then took turmeric powder because his aunt said it’s ‘anti-inflammatory.’ Three weeks later, he was in the hospital with kidney flare-up. No one told him turmeric’s a CYP3A4 inhibitor too. We need more folks like you, writing in plain talk. This isn’t just science-it’s survival. And if you’re on this med? You’re not just a patient-you’re a warrior. Keep fighting, keep asking, keep listening. We’re all in this together.
Katy Bell
I read this and just cried. Not because I’m scared-but because I’m grateful. My sister’s a transplant nurse, and she’s the reason I’m still here. She’s the one who caught the interaction between my cyclosporine and that ‘harmless’ antifungal cream. She didn’t just check a list-she looked me in the eye and said, ‘This isn’t worth the risk.’ I didn’t even know it was a risk. Thank you for writing this. It’s not just information-it’s a lifeline.
Lisa Lee
U.S. medical guidelines are so outdated. In Canada, we’ve had genetic testing standard for cyclosporine since 2019. Why are you still playing Russian roulette with your liver? You people need to stop being lazy and start demanding better care. This isn’t a blog-it’s a public health crisis. And yes, I’m calling you out.