Statin Symptom Checker: Myopathy vs. Neuropathy
What's Your Symptom?
This tool helps you determine if your symptoms are more likely related to statin-associated myopathy or neuropathy.
Remember: Never stop taking your statin without consulting your doctor.
This tool provides general guidance based on symptom patterns. For an accurate diagnosis, please consult your healthcare provider.
Many people on statins start noticing muscle cramps, aches, or tingling and immediately worry: is this the statin causing damage? The truth is, not all muscle discomfort from statins is the same. Two very different conditions can mimic each other - statin-associated myopathy and statin-related neuropathy. One affects your muscles directly. The other affects your nerves. Mixing them up can lead to the wrong treatment, unnecessary fear, or even stopping a life-saving medication when you don’t need to.
What Statin Muscle Cramps Really Look Like
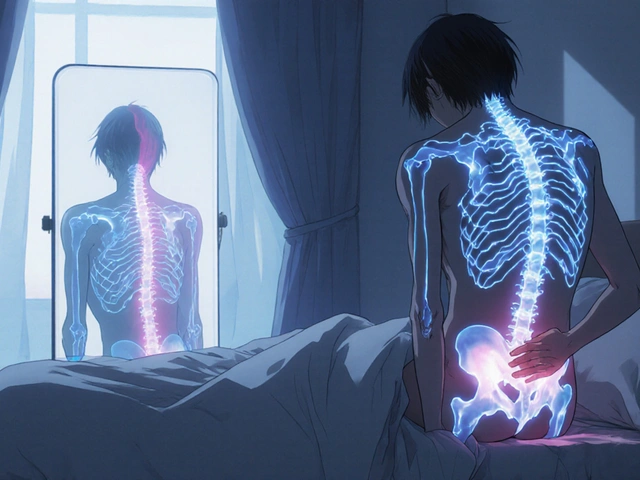
If you’ve been on a statin for a few weeks or months and suddenly feel tight, painful cramps in your thighs, hips, or shoulders - especially when climbing stairs or getting up from a chair - you’re not alone. About 7 to 29% of people on statins report some kind of muscle symptom, according to the European Atherosclerosis Society. But here’s the catch: most of these aren’t dangerous. True muscle damage, called myopathy, with dangerously high CK levels, happens in only about 1 in every 1,000 to 10,000 people. Statin myopathy usually feels like deep, dull aches in the large muscles near your trunk. It’s not sharp or localized like a pulled muscle. It’s more like your legs feel heavy, weak, or stiff. You might notice you’re slower walking uphill, or you need to use your arms to push yourself up from a low chair. Unlike exercise soreness, this doesn’t go away after a day or two. It lingers. And it’s often worse in the morning. What makes it tricky? Creatine kinase (CK), the enzyme doctors check to confirm muscle damage, is often only slightly elevated - or even normal - in most cases. That means a normal blood test doesn’t rule out myopathy. The real clue is timing: symptoms start after you begin the statin, get better when you stop it, and return if you restart it. That’s the gold standard for diagnosis.Why Statins Cause Muscle Problems
Statins block HMG-CoA reductase, an enzyme your liver uses to make cholesterol. But that same enzyme is also active in your muscles. Skeletal muscle is about 40 times more sensitive to this blockage than the liver, according to studies in mice. When statins interfere, they disrupt three key processes:- They reduce coenzyme Q10 (CoQ10) by up to 40% within a month. CoQ10 helps your muscles produce energy. Less of it means muscles tire faster.
- They interfere with protein prenylation, which messes with how muscle cells communicate and repair themselves.
- They throw off calcium balance inside muscle cells, leading to uncontrolled contractions - which is what causes cramps.
Neuropathy: When It’s Your Nerves, Not Your Muscles
Now imagine this: instead of heavy legs, you feel tingling, burning, or numbness in your feet - like you’re walking on pins and needles. The sensation creeps up your calves, like a sock being pulled tight. This isn’t muscle pain. This is neuropathy - nerve damage. Some people assume statins cause this too. But the evidence is messy. One 2021 review found some studies linking long-term statin use to peripheral neuropathy. Another study from 2019, looking at over 600 patients, found statin users were actually less likely to have neuropathy than non-users. The odds ratio was 0.5 - meaning statins might even be protective. How could that be? One theory is that statins lower LDL cholesterol, which carries vitamin E - a key antioxidant for nerve health. Less vitamin E might mean more nerve damage. But another theory says statins improve blood flow and reduce inflammation, which helps nerves. The truth? We don’t have a clear answer yet. Most experts agree: statin-induced neuropathy is possible, but it’s far from proven.
How to Tell the Difference
Here’s the practical guide to figuring out what’s really going on:| Feature | Statin Myopathy | Statin-Related Neuropathy |
|---|---|---|
| Symptom Location | Proximal muscles: thighs, hips, shoulders | Distal nerves: feet, ankles, hands |
| Symptom Type | Aching, weakness, cramping, heaviness | Tingling, burning, numbness, pins and needles |
| CK Levels | Often mildly to moderately elevated | Normal |
| Nerve Conduction Study | Normal | Reduced sensory nerve signals |
| Response to Stopping Statin | Improves in weeks to months | May not improve - symptoms may persist |
What to Do If You’re Having Symptoms
Don’t panic. Don’t quit your statin on your own. Here’s what works:- See your doctor and get a CK blood test. If it’s more than four times the normal level, that’s a red flag.
- Ask about a nerve conduction study if you have tingling or numbness. This is the only way to confirm neuropathy.
- Check for other causes: thyroid problems, vitamin B12 levels, alcohol use, or diabetes.
- If it’s myopathy and you need to stop the statin, try switching to a different one. Hydrophilic statins like pravastatin or rosuvastatin are less likely to cause muscle issues - about 60% of people who had trouble with one statin tolerate another.
- If symptoms don’t improve after 2-3 months off the statin, see a neurologist. Something else might be going on - and it wasn’t the statin at all.

Can You Stay on Statins?
Yes - if you need them. Statins cut your risk of heart attack and stroke by 25% for every 1 mmol/L drop in LDL cholesterol. That’s huge. Stopping them without a good reason can cost you years of life. If you have confirmed myopathy, your doctor can still get your cholesterol down. Use lower doses of a different statin, or add ezetimibe or a PCSK9 inhibitor. These non-statin drugs work differently and don’t cause muscle problems. In fact, the American College of Cardiology now says: if you’re statin-intolerant, don’t stop lipid-lowering therapy - just change how you do it.What About CoQ10 Supplements?
You’ve probably heard CoQ10 helps. It sounds logical - statins lower it, so take more back. But a 2015 JAMA study of 44 people with statin-related muscle pain found no benefit from CoQ10 compared to a placebo. Another trial in 2020 showed the same. So don’t waste your money. It’s not the magic fix.Final Thoughts
Muscle cramps on statins don’t automatically mean danger. Most are mild, reversible, and not caused by muscle destruction. But they also don’t mean you should ignore them. The key is knowing the difference between muscle and nerve problems - and acting based on facts, not fear. If you’re unsure, get tested. Don’t guess. Don’t stop your statin without a plan. And don’t assume every ache is the statin’s fault. Sometimes, the real problem was hiding in plain sight - and the statin was just the trigger that made it visible.Can statins cause permanent muscle damage?
In most cases, no. Statin-associated myopathy usually reverses within weeks to months after stopping the drug. Rarely, immune-mediated necrotizing myopathy can cause lasting damage, but this affects fewer than 1 in 100,000 users and requires specialized treatment like immunosuppressants. If symptoms persist beyond 3 months after stopping statins, see a neurologist to rule out other causes.
Is tingling in my feet a sign of statin neuropathy?
Possibly - but more likely it’s something else. Diabetes, vitamin B12 deficiency, and alcohol use are far more common causes of foot tingling. Statin-related neuropathy isn’t well proven. If you have this symptom, get your blood sugar and B12 levels checked first. A nerve conduction study can confirm if it’s neuropathy - but don’t assume it’s the statin.
Should I stop my statin if I have muscle cramps?
Not right away. Mild cramps are common and often harmless. Get a CK blood test and talk to your doctor. If your CK is normal and symptoms are mild, try switching to a different statin - like pravastatin or rosuvastatin - before quitting entirely. Stopping statins without a plan increases your heart attack risk.
Can I take CoQ10 to prevent statin muscle pain?
Studies haven’t shown it works. A 2015 JAMA trial found CoQ10 supplements provided no benefit over placebo for people with statin-related muscle symptoms. While it’s safe to take, don’t expect relief. Focus instead on switching statins or adding non-statin medications like ezetimibe if needed.
Are some statins less likely to cause muscle problems?
Yes. Hydrophilic statins like pravastatin and rosuvastatin are less likely to enter muscle cells, making them safer for people with muscle sensitivity. Simvastatin and atorvastatin, especially at high doses, carry higher risks. Genetic testing for the SLCO1B1 variant can also help - people with this gene are 4.5 times more likely to get muscle issues with simvastatin 80mg.
What if my muscle pain doesn’t go away after stopping statins?
If symptoms last longer than 2-3 months after stopping statins, you likely have another condition - like a nerve disorder, autoimmune disease, or thyroid problem. See a neurologist. They can run tests to find the real cause. Sometimes, statins unmask a hidden problem that was already there but silent.



Jennifer Walton
Statins are just another pharmaceutical illusion. We’ve been conditioned to believe cholesterol is the enemy, but nature never intended for us to live with synthetic inhibitors running our biochemistry. The body knows what it’s doing - even if the lab reports say otherwise.
Kihya Beitz
Oh great, another 10-page essay on why your muscles hurt but you still have to take the pill. 🙄 I’ve had cramps for 3 months, CK was normal, and my doctor just shrugged. Guess I’ll just keep walking like a robot.
Ogonna Igbo
In Nigeria we don’t have this problem because we don’t take these pills. Our grandmothers lived to 90 eating yam and palm oil. Now you people think you need a chemical to fix what your fast food destroyed. This is not medicine - this is corporate control disguised as science.
BABA SABKA
Let’s cut through the noise. Statin myopathy is a real biochemical cascade - CoQ10 depletion, calcium dysregulation, impaired prenylation. But neuropathy? The data’s too noisy. You’re conflating correlation with causation. The real villain here is the medical system’s inability to tolerate uncertainty. We need biomarkers, not anecdotes.
Chris Bryan
They’re not telling you the truth. Statins are a Trojan horse. The FDA knows they cause nerve damage. The pharmaceutical industry owns the studies. Look at the funding sources. CoQ10 is banned in Europe for a reason - it interferes with their profit margins. Wake up.
Jonathan Dobey
Here’s the existential truth: we’re all just meat sacks with faulty wiring, and statins are the cosmic glitch that makes us notice. The cramps? The tingling? They’re not symptoms - they’re the universe whispering, ‘You’ve been living in denial.’ We treat the cholesterol, not the soul’s dissonance. And that’s why no pill ever fixes what’s broken inside.
ASHISH TURAN
My father was on rosuvastatin for 8 years. He had mild cramps but never stopped. His CK was always normal. He’s 78 now, walks daily, no heart issues. The key is listening to your body - not the internet. If you feel off, talk to your doctor. Don’t self-diagnose based on Reddit threads.
Ryan Airey
Stop being so soft. If your muscles hurt, it’s because you’re weak. Statins aren’t the problem - your sedentary lifestyle is. Go lift something. Eat real food. Stop blaming Big Pharma for your lack of discipline. Also, CoQ10 is a scam. You’re wasting money.
Hollis Hollywood
I’ve been reading this whole thing and I just want to say - I get it. I’ve been there. I thought my cramps were the statin. I was terrified. I almost quit. But after talking to my cardiologist and getting a nerve study, turns out I had early diabetes. The statin was just the trigger. It’s scary to realize your body’s been screaming and you were too afraid to listen. Thank you for writing this. It helped me feel less alone.
Aidan McCord-Amasis
CoQ10 is a scam 😴📉
Adam Dille
Love this breakdown. So many people panic and quit statins. I’ve been on pravastatin for 5 years - zero issues. Switched from atorvastatin after mild cramps. Also, yes to checking B12 and thyroid. So many people miss that. 👏
Katie Baker
Thank you for writing this. I was so scared I was damaging my muscles. Got my CK tested - normal. Switched to rosuvastatin. Cramps are gone. You’re right - it’s not always the statin. Sometimes it’s just aging. But now I know what to look for. 😊
John Foster
The real tragedy isn’t statin myopathy - it’s the collapse of medical epistemology. We’ve replaced clinical wisdom with algorithmic diagnostics, and now we’re left with a generation that can’t distinguish between a biochemical perturbation and a metaphysical crisis. The body doesn’t lie - but the lab report does. The nerve conduction study? A mere shadow of the truth. What we’re witnessing is the fragmentation of the self under pharmacological surveillance. The cramps are a symptom of alienation - not just from cholesterol, but from the very rhythm of biological existence. And we call this progress?