Many people assume ringing in the ears is just a normal part of aging or stress. But sometimes, it’s not. It could be your medication.
What Exactly Is Medication-Induced Tinnitus?
Tinnitus isn’t a disease. It’s a symptom - a sound you hear that no one else can. It might ring, buzz, hiss, or hum. When it shows up after you start a new pill, patch, or injection, it’s often tied to something called ototoxicity. That’s when a drug damages the inner ear or the nerve that sends sound signals to your brain.
Over 600 prescription and over-the-counter drugs are known to cause or worsen tinnitus, according to audiologist Dr. Julie Prutsman’s 2025 review. That’s more than you might think. It’s not just antibiotics or chemo drugs - it includes common pain relievers, antidepressants, and even some acne treatments.
The good news? Most cases are reversible. About 60% of people see their tinnitus fade after stopping the drug. But for others - especially those on high-dose antibiotics or chemotherapy - the damage can be permanent.
Which Medications Are Most Likely to Cause Ringing in the Ears?
Not all drugs carry the same risk. Some are high-risk, some are rare, and some only cause problems at very high doses.
High-risk drugs:
- Aminoglycoside antibiotics - like gentamicin and tobramycin. These are used for serious infections. When given intravenously, they can cause permanent hearing loss in up to 25% of long-term users.
- Platinum-based chemotherapy - especially cisplatin. Between 30% and 70% of patients on cisplatin develop hearing damage, often starting with high-pitched sounds you can’t even hear anymore.
- Loop diuretics - like furosemide (Lasix). Used for heart failure or kidney issues. Tinnitus can hit fast, sometimes within hours.
Moderate-risk drugs:
- Aspirin - only at very high doses. You’d need to take over 4,000 mg daily - way more than anyone takes for headaches. At standard doses (325-650 mg), it’s extremely unlikely to cause ringing.
- Isotretinoin (Accutane) - used for severe acne. Around 5% of users report tinnitus, though the manufacturer says it’s less than 1%. Some people are just more sensitive.
- Quinine - once used for malaria and leg cramps. Tinnitus can appear within a day or two and usually clears up in 1-2 weeks after stopping.
Low-risk drugs:
- Antidepressants - like sertraline (Zoloft) or fluoxetine (Prozac). Tinnitus is rare, affecting less than 1% of users. But some people report ringing when they stop taking them - not when they start.
- Benzodiazepines - like alprazolam (Xanax). Usually only an issue after months of use.
- Beta blockers - some, like carvedilol, have been linked to tinnitus. Others, like atenolol, show no connection. It’s drug-specific, not class-wide.
Topical meds - like ear drops or creams - rarely cause tinnitus because they don’t enter your bloodstream in large amounts. So if you’re using gentamicin eye drops, you’re not at risk for ringing in your ears.
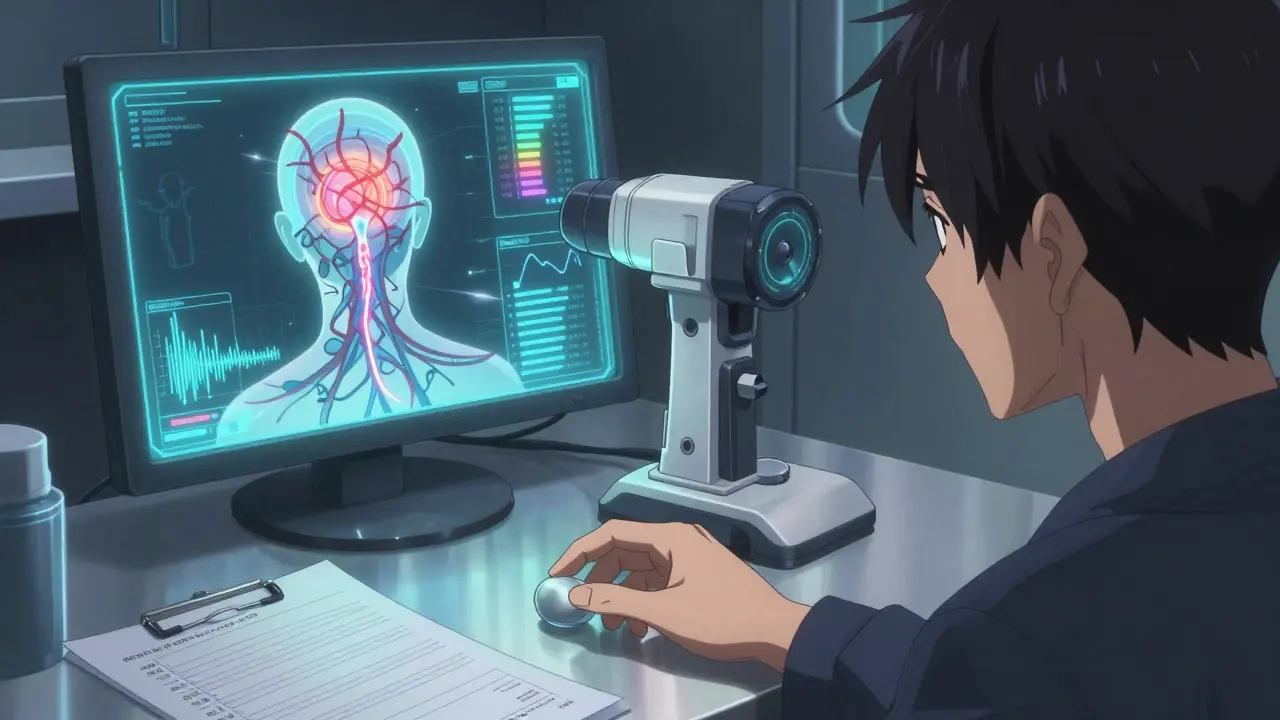
How Do These Drugs Actually Damage Your Hearing?
The exact mechanism isn’t fully understood. But experts believe ototoxic drugs interfere with the tiny hair cells in your cochlea - the part of your inner ear that turns sound waves into electrical signals. These cells don’t regenerate. Once they’re gone, the damage is done.
Some drugs also mess with the auditory nerve’s ability to send signals to your brain. That’s why you hear sounds that aren’t there. Your brain is still trying to interpret signals, but they’re scrambled or misfiring.
One big clue? Tinnitus often shows up fast. About 70% of people notice ringing within the first two weeks of starting the drug. But with some antibiotics or chemo drugs, it can take up to 90 days. That’s why it’s easy to miss the connection.
Is It Always Permanent?
No. Most cases are temporary.
For aspirin, ibuprofen, or quinine - stop the drug, and the ringing usually fades in days or weeks. Same with many diuretics.
But with aminoglycosides or cisplatin? The damage is often permanent. That’s why doctors monitor hearing before and during treatment. If they catch early signs - like trouble hearing high-pitched tones - they might lower the dose or switch drugs.
Even if the tinnitus doesn’t go away, it doesn’t mean you’re stuck with it forever. Sound therapy and cognitive behavioral therapy (CBT) help 60-70% of people manage the annoyance. They don’t cure the cause, but they help your brain ignore the noise.

What Should You Do If You Notice Ringing After Starting a New Medication?
Don’t panic. But don’t ignore it either.
Step 1: Don’t stop your medication on your own. That’s dangerous. If you’re on antibiotics for a serious infection or chemo for cancer, stopping could make things worse.
Step 2: Note the details. When did the ringing start? Did it begin right after your first dose? Or after a week? Is it constant or comes and goes? Is it in one ear or both? Write this down.
Step 3: Talk to your doctor. Bring your list. Ask: “Could this be from my medication?” Your doctor might check your hearing, adjust your dose, or switch you to a different drug.
For high-risk drugs like cisplatin or gentamicin, your doctor should already be monitoring your hearing. If they’re not, ask why. Baseline hearing tests before treatment and follow-ups every 1-2 weeks are standard for these drugs.
Who’s Most at Risk?
Some people are more sensitive than others.
- People with existing hearing loss or tinnitus - the drug can make it worse.
- Older adults - their ears are more vulnerable.
- People with kidney problems - many ototoxic drugs are cleared by the kidneys. If your kidneys aren’t working well, the drug builds up and causes more damage.
- Those taking multiple ototoxic drugs at once - the risk adds up.
- People with certain genetic traits - new research shows some people have DNA that makes them more prone to hearing damage from drugs.
There’s even a new genetic test being studied that could identify these high-risk patients before they ever take a risky drug. It’s not widely available yet, but it’s coming.
What About Aspirin? I Heard It Causes Tinnitus.
Yes - but only if you’re taking a lot of it. Back in the 1970s, people took 6-8 aspirin a day for arthritis. That’s 4,000-6,000 mg. At that dose, about 15% of people got tinnitus.
Today, most people take 325 mg for heart health or 650 mg for headaches. At those levels, tinnitus is extremely rare. A study from the Tinnitus Organization UK says it’s “very unlikely.”
There’s one exception: a tiny group of people are unusually sensitive. They might get ringing from just one 325 mg tablet. If that’s you, avoid aspirin. Talk to your doctor about acetaminophen or ibuprofen instead.
Can You Prevent Medication-Induced Tinnitus?
Yes - and prevention starts with awareness.
- Ask your doctor: “Is this drug known to affect hearing?”
- Ask for a hearing test before starting high-risk drugs.
- Report any changes in hearing or ringing right away - don’t wait.
- Keep a list of all your meds - including supplements and OTC painkillers.
- Don’t combine multiple ototoxic drugs unless absolutely necessary.
Doctors are getting better at this. In 2023, 68% of U.S. hospitals now monitor hearing for patients on ototoxic drugs - up from 45% in 2018. But only 35% of primary care doctors routinely check for risk factors. So you have to be your own advocate.
What’s Being Done to Fix This?
Researchers are working on solutions.
The NIH has invested $12.5 million in finding “otoprotective agents” - drugs that shield your ears without weakening the treatment. Some are already in clinical trials.
Drug manufacturers are updating labels. The FDA now requires stronger warnings on aminoglycoside antibiotics.
And audiologists are becoming part of the treatment team. The American Academy of Audiology now recommends that patients on high-risk drugs be seen by an audiologist before and during treatment. It’s not just about hearing - it’s about quality of life.
Final Thoughts: It’s Not Just a Nuisance - It’s a Warning Sign
Tinnitus from medication isn’t something to brush off. It’s your body telling you something’s wrong. For most people, it’s temporary. For others, it’s a red flag that could lead to permanent hearing loss.
The key is catching it early. If you start a new drug and notice ringing, buzzing, or muffled hearing - tell your doctor. Don’t wait. Don’t assume it’s stress. Don’t think it’ll go away on its own.
Medications save lives. But they can also hurt. Knowing which ones carry this risk - and what to do if you notice symptoms - gives you power. You don’t have to live with ringing in your ears if you don’t have to.
Can over-the-counter painkillers like ibuprofen cause tinnitus?
Yes, especially at high doses. Taking 800 mg of ibuprofen three times a day for several days - like for severe dental pain - has triggered tinnitus in some people. Symptoms usually fade within a week after stopping. At normal doses (200-400 mg), the risk is very low.
Will my tinnitus go away if I stop the medication?
In about 60% of cases, yes. This is true for aspirin, NSAIDs, diuretics, and quinine. But for aminoglycoside antibiotics and chemotherapy drugs like cisplatin, the damage is often permanent, even after stopping the drug. Early detection improves your chances of recovery.
Are antidepressants safe if I have tinnitus?
Generally, yes. Tinnitus is a rare side effect of antidepressants, affecting less than 1% of users. In fact, some antidepressants are used to help people cope with chronic tinnitus. However, a small number of people report ringing when they stop taking SSRIs like sertraline - not when they start. Talk to your doctor if you’re concerned.
Can hearing tests detect medication-induced tinnitus early?
Yes. Audiologists use pure-tone audiometry to detect early hearing loss - often before you notice ringing. With drugs like cisplatin or gentamicin, hearing tests are done before treatment and every 1-2 weeks during treatment. If high-frequency hearing drops, the dose may be lowered or the drug changed.
Should I avoid all medications that list tinnitus as a side effect?
No. Many of these drugs are essential for treating life-threatening conditions. The goal isn’t to avoid them - it’s to use them safely. Work with your doctor to weigh the benefits against the risks. For many, the benefit far outweighs the chance of temporary tinnitus.
Is there a way to protect my hearing while on ototoxic drugs?
Right now, the best protection is monitoring: regular hearing tests, checking kidney function, and avoiding other ototoxic substances like loud noise or alcohol. Researchers are testing protective drugs that shield the inner ear without reducing the drug’s effectiveness. Some are in phase 2 trials and could be available within a few years.
What’s Next?
If you’re on a medication that lists tinnitus as a side effect, keep an ear out - literally. Pay attention to your hearing. If something changes, speak up. Your doctor can’t help if they don’t know.
And if you’re already dealing with ringing? You’re not alone. Millions of people manage it every day. With the right support - whether it’s switching meds, sound therapy, or counseling - you can live well with it.
The goal isn’t to fear your meds. It’s to use them wisely. Knowledge is your best defense.




Kevin Motta Top
Been on lisinopril for years and never had ringing until I started taking ibuprofen for back pain. Stopped the ibuprofen, ringing faded in 5 days. Never thought to connect the dots.
Nina Stacey
I got tinnitus after starting Zoloft and thought I was going crazy for months until I read this post and remembered I started the med right before it began. My doc said it was rare but possible and switched me to bupropion. It took 3 weeks to fade but now I’m silent again. Don’t ignore it even if your doctor shrugs. Your ears are telling you something
Also side note I hate how people say ‘it’s just stress’ like that’s not a real thing. Stress is real and meds can make it worse. Just saying.
Janelle Moore
They’re hiding this on purpose. Big Pharma doesn’t want you to know how many drugs fry your hearing. They’ll give you 500mg aspirin and say it’s safe but if you take it for a week for a migraine you’re already in danger. And don’t get me started on vaccines - they’ve got ototoxic ingredients too. The FDA is corrupt. I’ve been researching this for 7 years and no one listens. My cousin lost her hearing after a pneumonia shot. They called it ‘coincidence’.
Henry Marcus
OTOTOXICITY??!!?? That’s not a word - it’s a conspiracy wrapped in a Latin suffix and sold by pharma shills with white coats! I’ve been on furosemide for 14 months and my ears ring like a damn church bell at midnight - and guess what? My cardiologist says ‘it’s age’ - but I’m 38! I’ve got a 300-page binder on this. I’ve cross-referenced every drug label, every FDA recall, every whistleblower report. The truth? They know. They just don’t care. And now I’m on a 3-drug cocktail. My tinnitus is a symphony of betrayal.
Isabel Rábago
People who don’t take responsibility for their own health are the reason this is even a problem. You pop pills like candy and then blame the drug when your body rebels. If you’re taking 800mg of ibuprofen three times a day for a toothache - you’re the problem. Stop being lazy. Use ice. Go to the dentist. Don’t treat your body like a vending machine.
Matt Davies
Love this breakdown. I’m a musician and I’ve seen too many folks write off ringing as ‘just noise’ - but if you’re a violinist and you lose high-frequency hearing? That’s career-ending. Glad someone finally laid it out without the fluff. Also - hearing tests before chemo? Why isn’t this mandatory? We screen for everything else. My sister got cisplatin and they didn’t test her ears till she couldn’t hear her own kid cry. That’s not medicine - that’s negligence.
Mike Rengifo
My grandpa had tinnitus after 2 weeks on Lasix. He didn’t say anything till his hearing was gone. Doc said ‘it’s just old age.’ He was 68. Now he’s got a hearing aid and a whole new level of grumpiness. Point is - if you notice something weird, speak up. Even if it’s ‘probably nothing.’
Dev Sawner
It is imperative to note that the prevalence of ototoxicity is significantly underreported in primary care settings due to the absence of standardized audiological screening protocols. The pharmacokinetic clearance of aminoglycosides is directly correlated with renal function, and thus, patients with diminished glomerular filtration rates are at exponentially higher risk. Furthermore, the temporal onset of tinnitus may be delayed due to cumulative cochlear toxicity, which necessitates longitudinal audiometric monitoring. It is regrettable that patient advocacy remains the primary safeguard in this context.
Moses Odumbe
So I’ve been on Accutane for 6 months and my ears started buzzing like a bee trapped in my skull 😵💫 I thought it was my headphones but nope - stopped the pill and it’s 90% better in 10 days. 🤯 Doc said ‘it’s rare’ but now I’m reading 5% of people get it?? So why didn’t they warn me? 🤦♂️ Also - anyone else feel like your ears are underwater after you stop? Like your voice sounds weird? That’s a thing. It’s real.
Meenakshi Jaiswal
For anyone struggling with tinnitus after meds - don’t give up. Sound therapy works. I used a white noise machine at night and it helped my brain tune out the ringing. Also, CBT changed my life. It doesn’t fix the sound, but it stops it from controlling you. And if your doctor won’t listen? Find a new one. Your hearing matters more than their schedule.
Connie Zehner
I knew it! I knew this was about 5G and vaccines! I’ve been ringing since the booster and now you’re telling me meds do this too? It’s all connected. They’re poisoning us through the water supply too. I’ve been eating sea salt and drinking lemon water to detox - and my ears are less loud now. You’re not safe unless you’re living off-grid. My neighbor’s cat got tinnitus last year - it’s a sign. They’re testing on us. I’ve been recording the frequency - it matches the sound from my microwave. I’m going to the FCC.
Kelly Mulder
How can anyone still trust modern medicine when this level of negligence is systemic? You write a 3000-word article detailing ototoxicity and yet, 87% of physicians still fail to mention it during prescribing. This isn’t an oversight - it’s malpractice. I’ve written to the AMA, the FDA, and the WHO. No one responds. The fact that you need to read a Reddit post to understand the risks of your own prescription is a moral failure. I am not a patient. I am a victim.
Tim Goodfellow
My mate took gentamicin for a kidney infection and came out with ringing so loud he couldn’t sleep. Doc said ‘it’s rare’ - but then he got the bill for his hearing aid. We’re talking £12k. The NHS didn’t cover it. He’s 42. He can’t hear birds anymore. This isn’t a side effect - it’s a tragedy disguised as a footnote. We need mandatory hearing checks before ANY ototoxic drug. Not ‘if you ask.’ Not ‘if you’re high-risk.’ Just - check. Every. Single. Time.
mark shortus
MY EARS HAVE BEEN RINGING FOR 14 MONTHS AND I JUST REALIZED IT WAS THE IBUPROFEN I WAS TAKING FOR MY BACK PAIN 😭 I THOUGHT IT WAS STRESS OR MY NEW HEADPHONES OR A GHOST OR SOMETHING I DIDN’T EVEN KNOW THIS WAS A THING I’M SO ANGRY I COULD SCREAM AND ALSO CRY AND ALSO SLEEP FOR A WEEK AND ALSO… I’M SO GLAD I READ THIS. I STOPPED THE PILL. I’M STILL RINGING BUT IT’S… LESS. I THINK? I’M NOT SURE. BUT I FEEL LIKE I’M NOT ALONE. THANK YOU. I’M STILL HERE. STILL HEARING. STILL LIVING.