Herbal supplements are plant‑derived products people turn to when they want relief from the unpleasant effects of prescription drugs, chemotherapy, or even everyday aches. While the word “natural” feels reassuring, the reality is messier - some herbs help, others hurt, and many sit somewhere in between. This guide pulls together the latest research, real‑world reports, and safety alerts so you can decide which remedies, if any, are worth trying for side‑effect management.
Why the "natural equals safe" myth falls apart
The National Center for Complementary and Integrative Health (NCCIH) reported that 23.2% of U.S. adults used natural products in 2012, a jump of nearly 18% from five years earlier. Yet the same period saw a surge in adverse‑event reports to the FDA, especially for herbs like Ephedra. A 1999 analysis of more than 800 cases linked Ephedra to heart attacks, strokes, and deaths, even at doses as low as 1 mg per day. JAMA’s 2016 review echoed this, listing severe reactions such as seizures, tachycardia, and liver failure across dozens of “herbal medicines.” In short, the safety record of many popular botanicals looks anything but flawless.
How to evaluate the evidence
When you’re hunting for a supplement to tame nausea, insomnia, or joint pain, ask three simple questions:
- Is there a peer‑reviewed clinical trial supporting the claimed benefit?
- What side‑effects have been documented, and how common are they?
- Does the herb interact with any of my prescription meds?
Answers can be found in databases like the Natural Medicines Comprehensive Database, the European Medicines Agency monographs, or reputable journals such as Nature and the American Journal of Family Physicians.
Top‑rated herbal options and what the data say
Below is a quick snapshot of five widely used supplements. The table follows a strict evidence‑grading system (high, moderate, low) based on the number of randomized trials, sample size, and consistency of outcomes.
| Herb | Typical Use | Evidence Strength | Common Side‑Effects | Key Interactions |
|---|---|---|---|---|
| Echinacea | Cold/flu symptom relief | Low - modest benefit in 2/5 trials | Rash, gastrointestinal upset | May boost immune response → caution with autoimmune drugs |
| Black cohosh | Menopausal hot flashes | Moderate - positive in 3/4 trials (formulation‑specific) | Headache, mild liver enzyme rise | Potential additive effect with hormonal therapies |
| St. John’s wort | Mild‑to‑moderate depression | High - 7/9 trials show benefit vs. placebo | Photosensitivity, GI discomfort | Induces CYP3A4 → reduces birth‑control, antidepressants, HIV meds |
| Ginkgo biloba | Memory support, circulatory health | Low - mixed results in 4/7 trials | Dizziness, headache | Increases bleeding risk with warfarin, aspirin, NSAIDs |
| Cranberry | UTI prevention | Moderate - 5/8 trials show modest reduction in recurrence | Stomach cramps, bitter taste | Potentiates anticoagulants → higher bleed risk |
When natural remedies can backfire
Even herbs with a solid evidence base can become hazardous when dosage, duration, or product quality slips. The Japanese Ministry of Health, Labour and Welfare recorded interstitial pneumonia in 1 in 25,000 users of a formula containing Scutellaria root (syo‑saiko‑to). Liver injury rates for many botanicals hover around 1‑5 per 10,000 users, with women over 50 most at risk. Contamination is another silent killer - heavy metals, pesticide residues, or outright adulteration with pharmaceutical agents have been uncovered in up to 37% of supplement batches tested by independent labs in 2022.
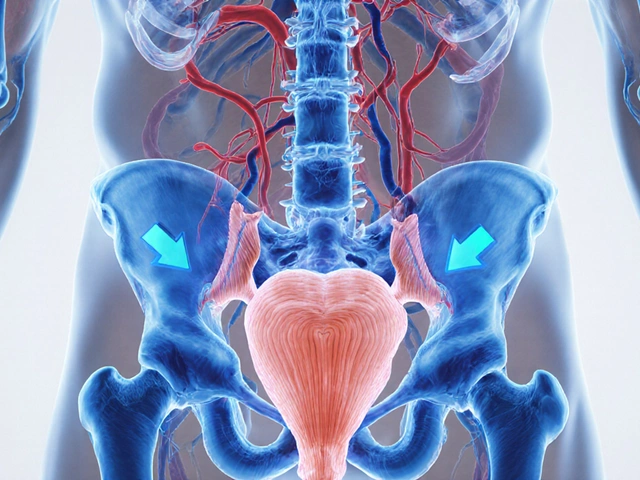
Special considerations for vulnerable groups
Older adults often have reduced renal and hepatic clearance, meaning the same herb can linger longer and amplify toxicity. JAMA highlighted that herbal elimination half‑lives can double in patients over 65, raising the odds of dizziness, falls, and organ stress. Pregnant or breastfeeding women should be especially cautious; St. John’s wort, for example, crosses the placenta and may affect fetal development.
People with chronic conditions such as heart disease, chronic kidney disease, or autoimmune disorders need a medication review before adding any supplement. The Mayo Clinic’s 2023 position paper stresses that “natural doesn’t always mean safe,” urging clinicians to ask patients about over‑the‑counter botanicals at every visit.
How to choose a quality product
When you’ve identified a herb that fits your symptom profile, the next hurdle is finding a trustworthy brand. Look for these hallmarks:
- Third‑party testing labels (USP, NSF, ConsumerLab)
- Transparent ingredient sourcing - manufacturers that disclose plant part, extraction method, and batch number
- Absence of proprietary blends that hide exact dosages
- Compliance with the European Medicines Agency’s monograph standards (if sold in the EU)
DNA barcoding, a technique introduced in the 2015 Botanical Adulterants Prevention Program, is becoming a gold‑standard for verifying species identity. If a brand mentions it, that’s a good sign.
Practical steps to integrate a supplement safely
- Consult your doctor or pharmacist. Share your full medication list, including over‑the‑counter drugs.
- Start with the lowest effective dose. Many side‑effects are dose‑dependent.
- Track symptoms daily for at least two weeks. Note any new aches, mood shifts, or lab value changes.
- If you’re on blood thinners, avoid high‑dose Ginkgo, cranberry, or garlic supplements unless your clinician approves.
- Report any serious reaction to the FDA’s Safety Reporting Portal; this helps build the evidence base.
Future outlook: tighter regulation and better research
Unlike pharmaceuticals, herbal supplements in the U.S. are not required to prove safety before hitting shelves, thanks to the Dietary Supplement Health and Education Act of 1994 (DSHEA). The European Medicines Agency, however, now mandates a monograph system that demands documented safety and traditional‑use evidence before a product can be marketed for a specific indication.
Researchers are pushing for larger, double‑blind trials. The NCCIH’s 2023 strategic plan earmarks $120 million for studies on long‑term herb safety, especially focusing on drug‑herb interactions. As more high‑quality data emerge, clinicians hope to shift the conversation from “are these herbs safe?” to “when are they beneficial, and for whom?”
Bottom line
Natural remedies can be powerful allies against medication‑induced side effects, but they come with their own set of risks. Evidence is strongest for a handful of herbs-St. John’s wort for mild depression and Black cohosh for menopausal hot flashes-yet even these demand careful dosing and monitoring. Always verify product quality, check for interactions, and keep your healthcare team in the loop.
Can I use Echinacea to treat chemotherapy‑induced nausea?
The evidence for Echinacea focuses on cold‑symptom relief, not chemotherapy side‑effects. Moreover, its immune‑stimulating properties could interfere with immunosuppressive cancer drugs. Talk to your oncologist before trying it.
Is Black cohosh safe for women with a history of breast cancer?
Current data suggest Black cohosh does not increase estrogen levels, but rare cases of liver enzyme elevation have been reported. Women with breast cancer should use only clinically tested preparations and do so under medical supervision.
How does St. John’s wort affect birth‑control pills?
St. John’s wort induces the liver enzyme CYP3A4, which can lower the blood levels of oral contraceptives by 15‑24%. Use a backup method (condoms or a copper IUD) while taking the herb.
Can Ginkgo biloba increase bleeding during surgery?
Yes. Ginkgo can inhibit platelet aggregation, so clinicians often ask patients to stop the supplement at least two weeks before any invasive procedure.
What should I look for on a supplement label?
Key items: exact ingredient (plant part and extraction ratio), amount per serving, batch number, third‑party certification, and a clear statement of any allergens or contaminants.



Abby W
Just tried a little cranberry extract after my last chemo session and felt a weird jitter in my hands 😬. Turns out the brand I grabbed wasn’t third‑party tested, so I’m now hunting for a certified batch.
Lisa Woodcock
That’s a solid reminder that not every “natural” label guarantees safety. When you’re navigating chemo side‑effects, it’s worth cross‑checking the supplement’s batch number with a third‑party lab report-something like USP or NSF can spare you the guesswork. Also, keep your oncologist in the loop; they can flag any potential herb‑drug interactions you might overlook.
Sarah Keller
When we speak of “natural” as a blanket term, we are really invoking a cultural myth that safety is inherent in the wild‑crafted, and that myth blinds both patients and clinicians to the brutal chemistry lurking in botanicals. The evidence base forces us to surrender romanticism and confront the fact that plant compounds interact with cytochrome enzymes in ways that are as predictable as a prescription drug’s pharmacokinetics. Consider St. John’s wort: a hyper‑active inducer of CYP3A4 that can shave half the plasma concentration of a birth‑control pill, a fact that has led to unintended pregnancies despite diligent use. Yet, the same herb delivers a clinically meaningful lift in depressive scores for a subset of patients, illustrating that efficacy and risk are two sides of the same coin. The responsibility, therefore, does not lie with the herb itself but with the framework we build around its deployment-rigorous dosing, transparent sourcing, and relentless monitoring. An aggressive stance is required: patients must log daily symptoms, labs must be rechecked when starting any new botanical, and clinicians need to enforce a zero‑tolerance policy for undocumented proprietary blends. Moreover, the research community must demand larger, double‑blind trials that stratify participants by age, comorbidities, and concurrent medications, lest we continue to sail by anecdote alone. In practice, this means asking three questions-do we have peer‑reviewed data, what adverse events are recorded, and how does it interact with my current regimen-before a single capsule touches the tongue. The cultural shift from “alternative” to “integrated” medicine hinges on this disciplined approach, and it is precisely the type of systemic rigor that can transform patient outcomes. Ignoring the nuance is not a neutral act; it is a negligent one that perpetuates harm under the guise of empowerment. Therefore, let us champion evidence, demand accountability, and keep the conversation grounded in both science and compassion. Patients who feel heard are more likely to adhere to monitoring protocols, creating a virtuous cycle of safety and efficacy. Healthcare systems must embed herbal review as a standard part of medication reconciliation, not an afterthought. Only then can we reconcile the ancient wisdom of botanicals with the rigor of modern medicine. In the end, the goal is not to vilify nature but to respect its power with informed stewardship.
kevin burton
For anyone hunting reliable brands, start by looking for USP, NSF, or ConsumerLab seals on the label-those certifications mean an independent lab has checked for contaminants and verified the listed potency. Also, prefer manufacturers that publish the exact plant part used (root, leaf, seed) and the extraction ratio; vague “proprietary blend” claims are a red flag.
Max Lilleyman
🙄 If you’re still buying supplements without those seals, you’re basically gambling with your health. The market is full of “natural” hype, and without third‑party verification you’re just taking a mystery powder.
Buddy Bryan
While third‑party testing is a solid benchmark, remember that even certified batches can vary batch‑to‑batch, especially with herbs prone to seasonal potency shifts. Keeping a simple log of how you feel after each dose can help you spot subtle changes that lab reports won’t capture.
Ken Dany Poquiz Bocanegra
Start low, go slow-most side‑effects are dose dependent.
krishna chegireddy
Don’t be fooled by the “low‑dose” marketing spiel; big pharma secretly funds many “natural” supplement trials to push products that keep patients dependent on costly drugs. The simplest way to stay safe is to question every claim and demand full transparency, even if it means buying a raw herb and testing it yourself.
Tamara Schäfer
I think its really importent to read the label carefully and also talk to your doctor before you start any new supplement, because they can help you avoid bad interactions and keep you feeling good.
Tamara Tioran-Harrison
Indeed, one would assume that medical professionals are universally eager to indulge in unsupervised herb experimentation, but alas, reality dictates that a brief conversation can prevent a cascade of iatrogenic mishaps. 😊
Charlie Stillwell
Bottom‑line: if the supplement isn’t FDA‑registered, treat it like a black‑box algorithm-unpredictable and potentially hazardous.