Mycophenolate Dose Reduction Calculator
Calculate Your Dose Adjustment
Dose reductions can significantly reduce nausea and diarrhea while maintaining effectiveness. Research shows 78% of patients see symptom improvement with a 33% dose reduction.
Your Recommended Dose Adjustment
Current Dose
Recommended Dose
What to Expect
With this reduction, 78% of patients experience symptom improvement within 72 hours. Your doctor should monitor blood levels to ensure effectiveness.
Important Notes
- This is a general guideline, not medical advice - Always discuss dose changes with your transplant team - Dose reduction should be done under medical supervision - Monitor for signs of rejection after adjustment
More than 1 in 3 people taking mycophenolate experience nausea or diarrhea. It’s not rare. It’s not unusual. It’s so common that doctors expect it. But that doesn’t make it easier to live with. If you’re on this medication after a transplant or for an autoimmune condition like lupus or vasculitis, you’re not just fighting your disease-you’re fighting your stomach too.
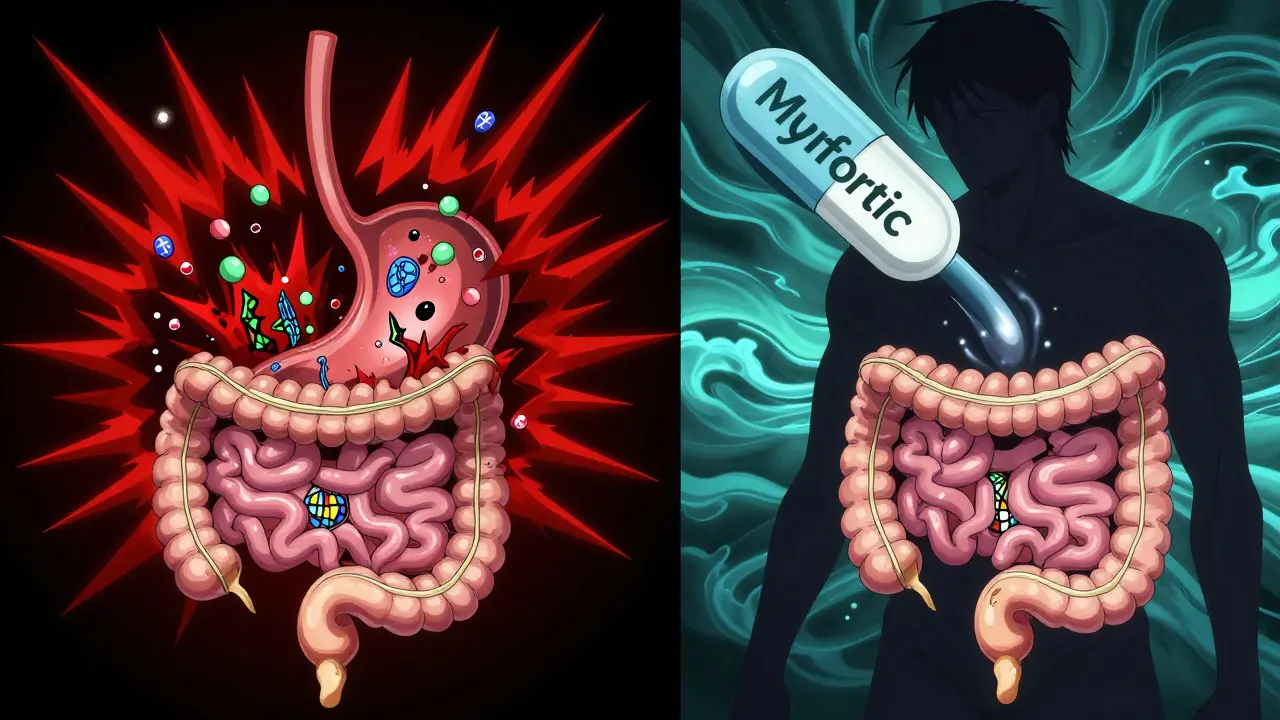
Why Does Mycophenolate Cause Nausea and Diarrhea?
Mycophenolate works by stopping immune cells from multiplying. That’s good for preventing organ rejection. But it doesn’t know the difference between immune cells in your kidney and immune cells in your gut. The lining of your intestines renews itself every few days. That rapid turnover makes it extra sensitive to drugs that block cell growth. When mycophenolate slows down this process, the gut lining breaks down faster than it can repair. That’s what leads to inflammation, irritation, and the classic symptoms: nausea, cramping, and loose stools.
The active part of the drug, mycophenolic acid (MPA), hits the gut hard right after you swallow the pill. That’s why nausea often hits within an hour. Diarrhea usually follows within a few hours or the next day. It’s not an infection. It’s not food poisoning. It’s the drug doing exactly what it’s supposed to do-just in the wrong place.
How Common Are These Side Effects?
Let’s get real about numbers. In clinical trials, about 31% of people taking mycophenolate had nausea. Nearly 30% had diarrhea. That’s not a small group. That’s almost one in three. In real-world settings, where people take it for years, the numbers climb even higher. One study of over 1,200 patients found that 63% reported GI problems. On Reddit, in a thread with nearly 300 transplant patients, over half said nausea or diarrhea made them consider quitting the drug.
And it’s not just mild. About 2% develop a serious form called mycophenolate-induced colitis-bloody diarrhea, severe cramps, fever. That’s not something you ignore. But for most, it’s just a daily grind: stomach upset, frequent trips to the bathroom, feeling tired, and anxious about leaving the house.
Dose Matters More Than You Think
The biggest mistake people make? Sticking with the full dose because they think “more is better.” It’s not. Mycophenolate’s side effects are strongly tied to how much is in your blood. When levels go above 3.5 μg/mL, diarrhea risk jumps over threefold. Many patients are on 1,000 mg twice a day-that’s 2 grams total. But research shows that dropping to 667 mg twice a day (a 33% reduction) resolves symptoms in 78% of people within 72 hours-without increasing rejection risk.
Doctors often hesitate to reduce the dose. They worry about rejection. But here’s the truth: you don’t need maximum suppression to stay protected. A lower dose, carefully monitored, still works. If your doctor hasn’t mentioned checking your MPA trough levels, ask. It’s not standard everywhere, but it should be.
Switching Formulations Can Be a Game-Changer
There are two versions of mycophenolate: mycophenolate mofetil (CellCept) and mycophenolate sodium (Myfortic). The main difference? Coating.
CellCept is a regular pill. It dissolves in your stomach. That’s why it causes so much upper GI upset. Myfortic is enteric-coated. It doesn’t break down until it hits the small intestine. That simple change cuts nausea and vomiting by nearly half in head-to-head studies.
A 2022 trial with 120 kidney transplant patients found that 65% of those who switched from CellCept to Myfortic saw their diarrhea and nausea improve enough to stay on the drug. If you’re struggling with nausea right after eating, switching could be your best move. Ask your pharmacist or transplant team if you’re on the right version.
When and How You Take It Makes a Difference
Timing isn’t just about convenience-it’s about control.
The official guideline says take it on an empty stomach: one hour before or two hours after food. That’s for maximum absorption. But if you’re throwing up every morning, that advice is useless.
Real-world advice from patients and clinicians? Take it with a small, low-fat snack. A few crackers. A spoonful of applesauce. A banana. One Reddit user said applesauce worked for 62% of the 48 people who tried it. Another said splitting the dose-taking half in the morning, half in the afternoon-cut their diarrhea from 5 times a day to 1 or 2.
Don’t take it with a big meal. Fats slow absorption and can make nausea worse. Avoid greasy food, dairy-heavy meals, or heavy sauces. Keep it simple. Toast. Rice. Plain yogurt.
Probiotics Might Help-But Not All of Them
Not every probiotic works. But some do. The strain Lactobacillus GG (found in Culturelle) has been studied specifically for mycophenolate-induced diarrhea. In one small trial, 49% of users reported improvement. That’s not a cure, but it’s enough for many to feel like they have some control.
Don’t waste money on multi-strain blends unless they include Lactobacillus GG. Avoid probiotics with added sugars or artificial flavors-they can make diarrhea worse. Stick to plain, refrigerated capsules. Take them at least two hours apart from your mycophenolate dose.

When to Worry: Red Flags You Can’t Ignore
Not every stomach ache means you need to stop the drug. But some signs mean you need to act fast:
- Diarrhea lasting more than 7 days
- Bloody or black stools
- Fever over 100.4°F (38°C)
- Severe abdominal pain
- Weight loss or dehydration (dry mouth, dizziness, dark urine)
If you have any of these, call your transplant team immediately. You could have mycophenolate-induced colitis-or worse, an infection like C. diff or CMV. These can look the same but need totally different treatment. A colonoscopy with biopsy is the only way to tell the difference. Don’t wait. Don’t assume it’s just the drug.
What If Nothing Works?
For about 14% of patients, mycophenolate side effects are just too much. They have to stop. And that’s okay.
There are alternatives. Azathioprine is older, less effective, but gentler on the gut. Leflunomide is newer and shows promise for people who can’t tolerate mycophenolate. It’s not perfect-it has its own side effects-but for some, it’s a better trade-off.
And now, there’s good news: a new extended-release version of mycophenolate (MPA-ER) was approved in early 2023. In trials, it cut diarrhea by 37% compared to the old pill. It’s not widely available yet, but if your doctor hasn’t mentioned it, ask. It could be the solution you’ve been waiting for.
Long-Term Outlook: Can You Stay on This Drug?
Mycophenolate is still the most-used immunosuppressant in transplants worldwide. Why? Because it works better than anything else at preventing rejection. Even with nausea and diarrhea, most people find a way to make it work.
It usually takes 3 to 6 months to get used to the side effects. Many patients say it gets better over time. Your body adjusts. Your dosing gets fine-tuned. You learn what foods help, what to avoid, when to take it. You become your own expert.
But you need support. Make sure your care team includes a transplant pharmacist. Ask for written guidelines. If your hospital doesn’t give you dietary tips, ask for them. You’re not asking for extra help-you’re asking for the standard of care.
And remember: your quality of life matters just as much as your lab numbers. If you’re too sick to work, to see your kids, to leave the house-you’re not succeeding just because your kidney is fine. You need to feel well, too.
There’s no shame in adjusting. There’s no shame in switching. There’s no shame in asking for help. This drug saves lives. But it shouldn’t steal yours.
Can I take mycophenolate with food if it causes nausea?
Yes, if nausea is a problem, taking mycophenolate with a small, low-fat snack like crackers, toast, or applesauce can help. Avoid large meals or fatty foods, which can worsen symptoms. While the drug is best absorbed on an empty stomach, many patients find that a light snack reduces nausea without significantly affecting absorption.
Is diarrhea from mycophenolate dangerous?
Mild diarrhea is common and usually not dangerous. But if it lasts more than 7 days, is bloody, or comes with fever or severe pain, it could be mycophenolate-induced colitis or an infection like C. diff. These require urgent medical attention. Always get checked if symptoms worsen or don’t improve with dose changes.
Should I switch from CellCept to Myfortic?
If you’re having frequent nausea or vomiting, switching from mycophenolate mofetil (CellCept) to mycophenolate sodium (Myfortic) is often helpful. Myfortic has an enteric coating that delays release until it reaches the small intestine, reducing upper GI irritation. Studies show 65% of patients see improvement after switching.
Can probiotics help with mycophenolate-induced diarrhea?
Yes, but only specific strains. Lactobacillus GG (found in Culturelle) has shown benefit in clinical studies, with nearly half of users reporting reduced diarrhea. Avoid multi-strain or sugary probiotics. Take them at least two hours apart from your mycophenolate dose.
What if I can’t tolerate mycophenolate at all?
If side effects are unbearable, alternatives exist. Azathioprine is older but gentler on the gut. Leflunomide is a newer option with promising results. A new extended-release mycophenolate (MPA-ER) also reduces diarrhea by 37%. Talk to your transplant team-stopping isn’t failure; finding a better fit is part of care.




Christi Steinbeck
I was on CellCept for 3 years and thought I was just a wimp until I switched to Myfortic-life changed. No more vomiting after breakfast. Just plain toast and coffee, and I could actually leave the house. If you’re struggling, just ask. No shame in asking for a coating.
Also, Lactobacillus GG? Game. Changer. Culturelle. Plain. Refrigerated. Two hours before my pill. Done.
Josh Kenna
yo i took 2g a day for 18 months and my doc never checked my mpa levels. i was having 8 diarrhea runs a day. turned out my blood level was 5.8. they dropped me to 667mg twice and now i’m fine. why is this not standard? why do we have to google this stuff ourselves? doctors are lazy. i’m not mad, just disappointed.
Erwin Kodiat
It’s wild how something so life-saving can also make you feel like you’re constantly fighting your own body. I used to dread mornings. Now I take my pill with a banana and a spoonful of almond butter. Doesn’t fix everything, but it makes the day feel less like a battle. You’re not broken. You’re just adjusting. And that’s okay.
Also, MPA-ER is coming. I heard it’s in 3 hospitals near me already. Keep asking. They’ll listen if you keep asking.
sujit paul
Let me be clear: this is not medicine. This is corporate manipulation. Mycophenolate was designed to be profitable, not tolerable. The enteric coating? That was invented after they realized people were dropping out. The ‘lower dose’ studies? Funded by the same companies that sell the pills. You’re being conditioned to accept suffering as normal. Wake up. Ask for azathioprine. It’s cheaper. It’s older. And yes-it’s gentler. The system doesn’t want you to know this.
Aman Kumar
It’s obvious that the pharmaceutical-industrial complex has weaponized immunosuppression. Mycophenolate is not a drug-it’s a control mechanism. The gut is the second brain, and by targeting its regenerative capacity, they’re not just suppressing immunity-they’re suppressing autonomy. The fact that you’re being told to ‘just take it with applesauce’ is a symptom of a deeper pathology. You are not a patient. You are a data point. And your suffering? It’s monetized.
Jake Rudin
...and yet, despite all this-the nausea, the diarrhea, the fear, the uncertainty-we’re still here. Still taking it. Still fighting. Because we know, deep down, that the alternative is worse. The kidney fails. The transplant dies. The body gives out. So we swallow the pill. We eat the crackers. We wait. We endure. And we do it again tomorrow. Not because we’re brave. But because we have no other choice. And that’s the quietest kind of courage there is.
Lydia H.
My mom’s on mycophenolate for lupus. She used to cry after dinner because she couldn’t keep anything down. We tried everything-peppermint tea, ginger chews, even acupuncture. Nothing worked until we switched to Myfortic. Now she bakes cookies on Sundays again. It’s not glamorous. But it’s enough. Don’t give up on the small wins.
Valerie DeLoach
For those asking about probiotics: Lactobacillus rhamnosus GG (ATCC 53103) is the only strain with peer-reviewed evidence for mycophenolate-associated diarrhea. Other strains, even within the Lactobacillus genus, lack sufficient data. Avoid products with inulin, fructooligosaccharides, or artificial sweeteners-they can exacerbate osmotic diarrhea. Refrigeration is non-negotiable; viability drops 50% after 30 days at room temperature. Take two hours before or after dosing. Consistency matters more than dose.
Jacob Hill
Wait-so if I take it with a banana, I’m not absorbing as much? I’ve been doing that for months…
Also, is it true that grapefruit juice makes it worse? I read that somewhere…
Christi Steinbeck
Nope, banana’s fine. It’s fats and big meals that slow absorption. A banana’s mostly carbs and fiber-actually helps the pill pass through without irritating the stomach lining. Grapefruit? Yeah, avoid it. It messes with liver enzymes that metabolize MPA. You don’t want higher blood levels. Trust me-I learned that the hard way.
Lewis Yeaple
According to the 2021 American Journal of Transplantation guidelines, the therapeutic window for mycophenolic acid is 1.0–3.5 μg/mL. Levels exceeding 3.5 μg/mL correlate with a 3.2-fold increase in gastrointestinal toxicity (p < 0.001). Therefore, dose reduction to 1,334 mg/day is not only acceptable but evidence-based. Failure to monitor trough levels constitutes a deviation from standard of care. Please consult your transplant pharmacist immediately.
Jackson Doughart
I used to hate this drug. Hated the way it made me feel. The constant dread. The bathroom anxiety. The guilt of feeling like I was letting everyone down because I couldn’t ‘just push through.’
Then I met another transplant patient at the clinic who told me: ‘You’re not weak for needing help. You’re smart for asking for it.’
That changed everything.
I asked for the MPA test. I switched to Myfortic. I started taking Culturelle. Now I’m hiking again. Not because I’m cured-but because I finally stopped trying to suffer in silence.