When your doctor prescribes Amoxil (amoxicillin), you might wonder: is this really the best option? Maybe you’ve heard about other antibiotics like cephalexin or azithromycin and started questioning if there’s something better-or safer-for your infection. You’re not alone. Many people look for alternatives because of side effects, past bad experiences, or just wanting to make sure they’re getting the most effective treatment. The truth? Not all antibiotics are created equal, and the right choice depends on what you’re treating, your medical history, and even your body’s reaction to drugs.
What Amoxil Actually Does
Amoxil is the brand name for amoxicillin, a penicillin-type antibiotic that’s been used since the 1970s. It works by stopping bacteria from building their cell walls, which kills them or stops them from multiplying. It’s effective against a wide range of common infections: strep throat, ear infections, sinus infections, urinary tract infections, and some types of pneumonia. It’s often the first choice because it’s cheap, well-studied, and usually gentle on the stomach compared to other antibiotics.
But here’s the catch: amoxicillin only works on bacteria. It does nothing for colds, flu, or most sore throats caused by viruses. Still, it’s prescribed often because doctors can’t always tell right away whether an infection is bacterial or viral. That’s why some people end up taking it unnecessarily-and that’s part of why antibiotic resistance is growing.
Common Alternatives to Amoxil
If you can’t take amoxicillin-or it didn’t work for you-there are several other antibiotics doctors turn to. Each has strengths, weaknesses, and risks. Here are the most common ones:
- Cephalexin (Keflex) - A cephalosporin antibiotic. Works similarly to amoxicillin but is often used when someone has a mild penicillin allergy. It’s good for skin infections, bone infections, and respiratory issues.
- Azithromycin (Zithromax) - A macrolide antibiotic. Often used for respiratory infections, especially when amoxicillin fails. Popular for its short 5-day course. Less likely to cause diarrhea than amoxicillin.
- Ciprofloxacin (Cipro) - A fluoroquinolone. Stronger, used for more serious infections like complicated UTIs or certain types of pneumonia. Not usually a first choice because of serious side effects like tendon damage and nerve issues.
- Clindamycin - Used for skin infections, dental abscesses, or when someone has a true penicillin allergy. Can cause severe diarrhea (C. diff infection), so it’s reserved for cases where other options won’t work.
- Doxycycline - A tetracycline antibiotic. Often used for acne, Lyme disease, or tick-borne illnesses. Not for kids under 8 or pregnant women because it affects bone and tooth development.
When to Choose Cephalexin Over Amoxil
If you’ve had a mild reaction to penicillin-like a rash that went away on its own-your doctor might switch you to cephalexin. About 10% of people who think they’re allergic to penicillin actually aren’t. But if you’ve had swelling, trouble breathing, or anaphylaxis, then cephalexin is a safer bet.
Cephalexin is just as effective as amoxicillin for ear infections and skin infections like cellulitis. One study in the Journal of the American Academy of Dermatology found no difference in cure rates between the two for skin infections. But cephalexin is taken less often per day (every 6-12 hours vs. every 8 hours for amoxicillin), which some people find easier to stick with.
Downside? Cephalexin can still cause diarrhea, and it’s not as effective against some strains of bacteria that amoxicillin handles well, like certain types of strep.
Azithromycin: The Short-Course Option
Azithromycin is famous for its 5-day course-sometimes even a single dose. That’s why it’s often called the "Z-Pak." It’s convenient, and many people prefer it because they don’t have to remember to take pills three times a day.
It’s particularly useful for bronchitis or sinus infections when amoxicillin didn’t help. It also works well for whooping cough and some sexually transmitted infections. But here’s the problem: azithromycin is overused. In the UK, NHS data shows it’s prescribed more than necessary for viral coughs. Overuse leads to resistance, meaning it won’t work as well when you really need it.
Also, azithromycin can affect heart rhythm in people with existing heart conditions. If you’ve had irregular heartbeat or are on heart medication, ask your doctor before taking it.

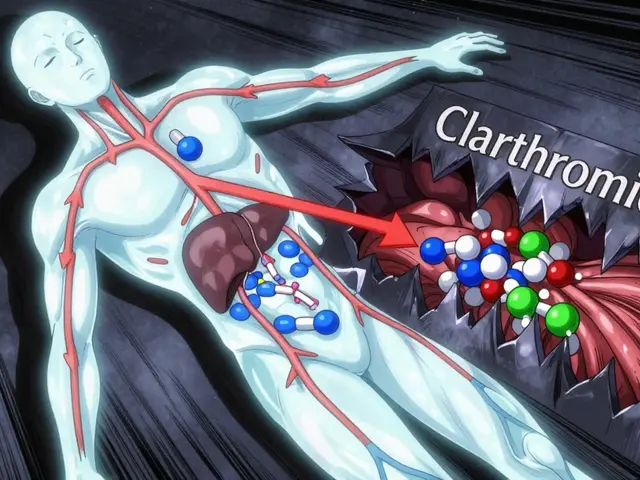
Clindamycin: Strong But Risky
Clindamycin is a powerful antibiotic that’s usually reserved for when other options fail. It’s great for dental abscesses, severe skin infections, and infections caused by MRSA. But it’s also one of the leading causes of a dangerous condition called Clostridioides difficile (C. diff) infection.
C. diff causes severe, watery diarrhea, stomach cramps, and fever. In older adults or people who’ve been on antibiotics before, it can be life-threatening. One study from the CDC found that people taking clindamycin were 17 times more likely to get C. diff than those taking amoxicillin.
So while it’s a solid backup, it’s not something you want to take unless you absolutely have to.
Why Amoxil Still Wins for Most People
Despite all the alternatives, amoxicillin remains the top choice for a reason. It’s broad-spectrum, meaning it covers many common bacteria. It’s affordable-often under £5 for a full course in the UK. It’s safe for kids, pregnant women, and older adults. And it’s well-tolerated: most people have no side effects beyond mild stomach upset or a rash.
Compared to ciprofloxacin or clindamycin, amoxicillin has far fewer serious risks. It doesn’t damage tendons, nerves, or gut flora as badly. It’s also less likely to cause yeast infections in women, though that can still happen.
The only real downsides? It doesn’t work against all bacteria (like some resistant strains), and it can’t be used if you have a true penicillin allergy. If you’ve had a reaction before, don’t guess-get tested. Many people think they’re allergic because they had a rash as a child, but only 1 in 10 are truly allergic.
Side Effects: What to Watch For
All antibiotics come with risks. Here’s what you might experience:
- Amoxicillin: Diarrhea (10-15% of users), nausea, vaginal yeast infection, rash (especially in people with mononucleosis).
- Cephalexin: Similar to amoxicillin, but slightly more likely to cause vomiting.
- Azithromycin: Stomach pain, nausea, less diarrhea than amoxicillin, but possible heart rhythm changes.
- Clindamycin: Severe diarrhea (C. diff), metallic taste, severe rash.
- Ciprofloxacin: Tendon rupture (especially in older adults), nerve pain, dizziness, sun sensitivity.
If you get watery or bloody diarrhea, severe stomach cramps, or a rash that spreads after starting any antibiotic, stop taking it and call your doctor. Don’t wait.
How to Decide What’s Right for You
There’s no one-size-fits-all answer. Here’s how to think about it:
- What’s the infection? Amoxicillin works best for ear, sinus, and mild lung infections. Azithromycin is better for bronchitis. Clindamycin is for skin or dental infections.
- Do you have allergies? If you’re truly allergic to penicillin, avoid amoxicillin and cephalexin. Ask for a penicillin allergy test.
- Have you taken antibiotics recently? If you’ve used clindamycin or ciprofloxacin in the last 6 months, your gut bacteria may already be disrupted. Amoxicillin is usually safer.
- How long can you take it? If you struggle to remember doses, azithromycin’s short course might help. But don’t choose it just for convenience.
- Are you pregnant or over 65? Amoxicillin is safest for pregnancy. Avoid ciprofloxacin and doxycycline.
Bottom line: Amoxil is still the go-to for most common infections. Alternatives exist, but they’re not necessarily better-just different. The best antibiotic is the one that matches your infection, your body, and your history.
Frequently Asked Questions
Can I take amoxicillin if I’m allergic to penicillin?
No. If you’ve had a true penicillin allergy-like swelling, trouble breathing, or anaphylaxis-you should avoid amoxicillin. But many people who think they’re allergic aren’t. A simple skin test can confirm it. If you had a rash as a child, ask your doctor about getting tested before assuming you can’t take it.
Is cephalexin stronger than amoxicillin?
Not necessarily. Cephalexin and amoxicillin cover similar types of bacteria, but they work slightly differently. Cephalexin is often used when someone can’t take penicillin, not because it’s stronger. For most common infections like ear infections or skin boils, they’re equally effective.
Why does my doctor prescribe azithromycin instead of amoxicillin for a cough?
Some coughs, especially bronchitis, are caused by bacteria that don’t respond well to amoxicillin. Azithromycin works better against those strains. It’s also used when the infection is likely to be atypical, like from mycoplasma or chlamydia. But many coughs are viral, and neither antibiotic helps-so make sure your doctor has ruled out a virus first.
Can I switch from amoxicillin to another antibiotic if I have side effects?
Yes, but don’t switch on your own. If you get diarrhea, rash, or nausea, contact your doctor. They might suggest stopping, switching, or adding a probiotic. Never stop antibiotics early just because you feel better-this leads to resistant bacteria. But if side effects are severe, your doctor can adjust your treatment.
Are natural alternatives like garlic or honey effective instead of antibiotics?
Honey can help soothe a sore throat, and garlic has mild antibacterial properties, but neither can replace antibiotics for bacterial infections like pneumonia, strep throat, or UTIs. Relying on them instead of prescribed antibiotics can lead to serious complications. Antibiotics are necessary when bacteria are causing harm-natural remedies aren’t strong enough to kill them.
What to Do Next
If you’ve been prescribed Amoxil and are unsure, ask your doctor: "Why this one? Are there other options?" If you’ve had side effects before, bring up your history. If you’re worried about resistance, ask if a test (like a rapid strep test or urine culture) could confirm the need for antibiotics.
Most importantly: take your full course. Even if you feel better in two days, finish all the pills. Stopping early is the #1 reason antibiotics stop working over time.
Amoxil isn’t perfect, but for most people, it’s still the best starting point. Alternatives exist for specific cases-but they’re not upgrades. They’re backups. Choose wisely, and always let your doctor guide you based on your body-not your Google search.





Cameron Daffin
Man, I love how this breaks down the antibiotics like a menu at a fancy restaurant-each one with its own vibe and risks. I had amoxicillin for a sinus infection last year and thought I was gonna die from the diarrhea, but honestly? Better than the alternative of untreated bacteria crawling through my sinuses. 😅
Carlo Sprouse
While the article presents a reasonable overview, it fails to address the systemic issue of pharmaceutical marketing influencing prescribing patterns. Amoxicillin is prescribed not because it's optimal, but because it's profitable, widely available, and requires minimal diagnostic precision. The medical community’s reliance on empirical treatment, rather than rapid diagnostics, perpetuates resistance. This is not a pharmacological issue-it's a structural one.
Carl Lyday
Just wanted to add a real-world note: I’m a nurse in rural Nebraska, and we’ve seen a huge spike in C. diff cases since clindamycin got pushed for dental abscesses in older patients. We now have a strict protocol: if the patient’s over 60 and has taken any antibiotic in the past 6 months, we avoid clindamycin unless it’s a last resort. Amoxicillin’s still the MVP for most cases-cheap, safe, and effective. Don’t overcomplicate it unless you have to.
Tom Hansen
amoxil is just penicillin but with a fancier name and higher price. doctors love it because its easy and they dont have to think. azithromycin is the real z-pak flex. also why is no one talking about how cipro can wreck your tendons? i know a guy who ran a marathon after taking it and snapped his achilles. lol
Kristen Magnes
For anyone reading this and feeling overwhelmed-your doctor isn’t trying to confuse you. They’re trying to match the right tool to the job. If you’re worried about side effects or resistance, bring this article to your next appointment. Ask: ‘What’s the evidence for this choice?’ You’re not being difficult-you’re being empowered. And that’s a good thing.
Donna Hinkson
I’ve been on both amoxicillin and cephalexin. The only real difference I noticed was that cephalexin made me feel slightly more nauseous. Otherwise, both cleared up my ear infection. I think the key is listening to your body and not assuming one is ‘better’-just different.
Rachel M. Repass
There’s a deeper epistemological layer here: we treat antibiotics as discrete solutions rather than ecological interventions. Each pill doesn’t just kill bacteria-it reshapes the microbiome’s evolutionary trajectory. The real question isn’t ‘which antibiotic?’ but ‘what are we willing to sacrifice in the microbial ecosystem for short-term relief?’ Amoxicillin is the least destructive option, yes-but we’re still playing with fire. We need to stop seeing infection as an enemy to eradicate, and start seeing it as a signal of imbalance.
Sharron Heath
Thank you for presenting this information with such clarity. I appreciate the emphasis on distinguishing between true penicillin allergies and childhood rashes. Many patients self-diagnose allergies without testing, leading to unnecessary avoidance of first-line therapies. A simple allergy evaluation can prevent overuse of broader-spectrum agents like clindamycin or fluoroquinolones, which carry greater risks. This is public health education at its best.
Arthur Coles
Let’s be real-Big Pharma is pushing azithromycin because it’s a 5-day course. They make more money selling you five pills than three. And don’t get me started on how cipro was pulled from the market in Europe but still sold here. They know about the tendon damage. They’ve known for 20 years. Your doctor isn’t your friend. They’re paid to prescribe. Always ask: ‘What’s the cheapest, safest option?’ and then go research it yourself.
Steve Dressler
As someone who’s had three rounds of antibiotics in five years, I’ve learned one thing: never assume your body reacts the same way twice. I took amoxicillin for a UTI and had zero issues. Then I took it for a sinus infection and broke out in hives. Turned out it was mononucleosis masquerading as strep-amoxicillin causes rashes in mono cases. So yes, context matters. Ask your doc for a rapid test. If they refuse? Get a second opinion. Your gut (literally) is worth it.