What Deep Brain Stimulation Actually Does for Parkinson’s
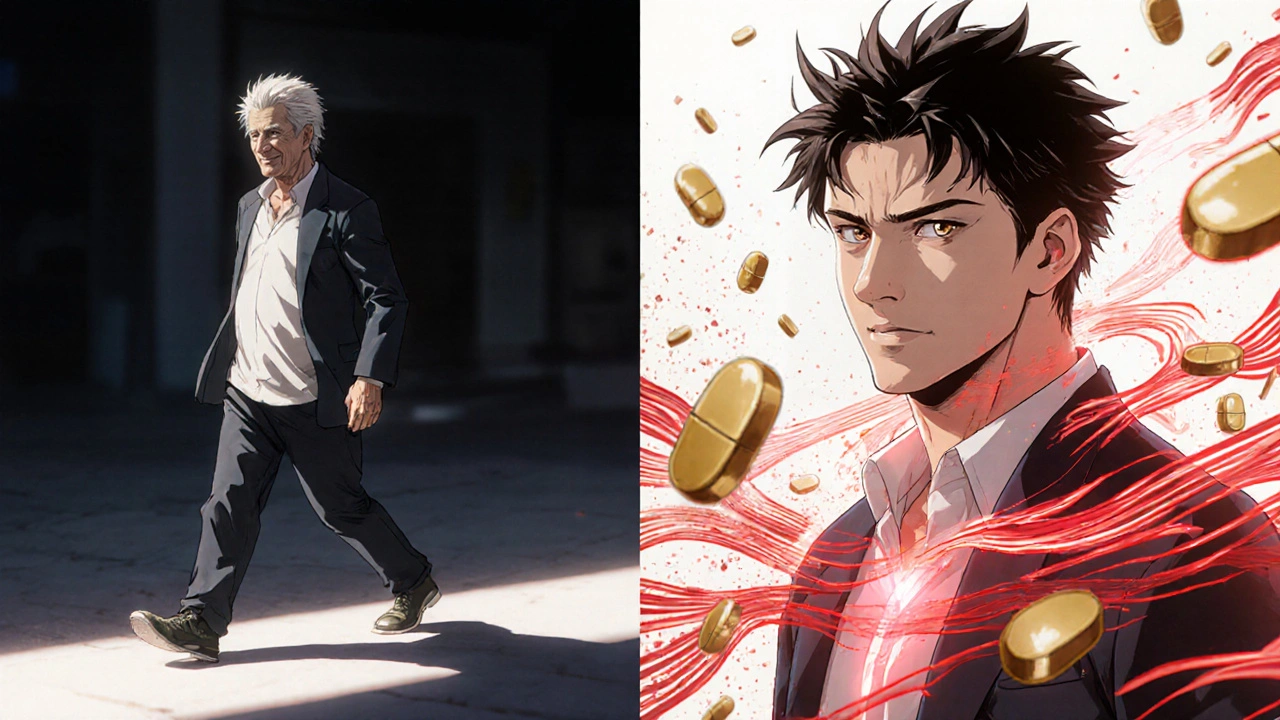
Deep Brain Stimulation, or DBS, isn’t a cure for Parkinson’s. It doesn’t stop the disease from progressing. But for many people, it changes everything. If you’ve been on levodopa for years and now find yourself stuck in OFF periods-where meds don’t work and movement feels frozen-DBS can cut those episodes by 60 to 80%. It can slash the wild, twisting movements called dyskinesias by up to 80%. And it often lets you cut your daily pill dose by 30 to 50%.
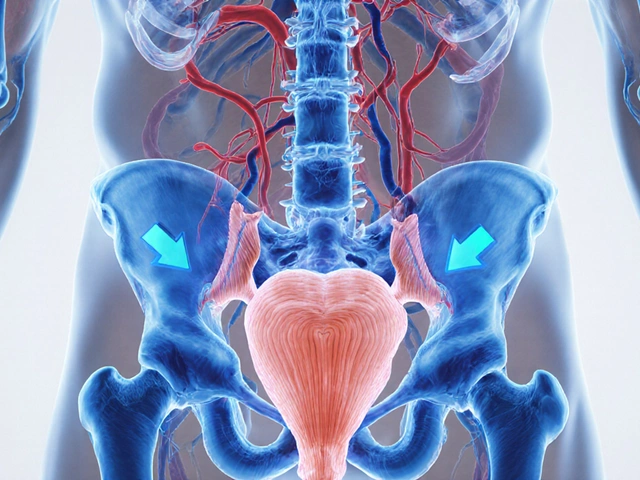
The procedure sends tiny electrical pulses to specific spots deep in the brain, like the subthalamic nucleus (STN) or the globus pallidus interna (GPi). These areas go haywire in Parkinson’s, firing signals that make your muscles stiff, slow, or shake uncontrollably. The pulses don’t destroy tissue. They don’t remove anything. They just calm the noise. Think of it like a pacemaker for your brain, but instead of regulating heartbeat, it smooths out the signals that control movement.
Modern systems like Medtronic’s Percept™ PC and Boston Scientific’s Vercise™ Genus™ can even sense brain activity in real time. They detect abnormal beta wave patterns (13-35 Hz), which spike during stiffness and slowness, and adjust stimulation automatically. This isn’t science fiction-it’s FDA-approved and in use right now. Patients report waking up feeling like they did 10 years ago: able to button shirts, walk without shuffling, and get out of bed without waiting for meds to kick in.
Who Is a Good Candidate for DBS?
Not everyone with Parkinson’s benefits from DBS. In fact, only about 1 to 5% of eligible patients ever get it-mostly because they’re never referred, or they wait too long.
The gold standard for screening comes from the CAPSIT-PD guidelines from 1999, still used today. To qualify, you need:
- A confirmed diagnosis of idiopathic Parkinson’s disease (not atypical parkinsonism like PSP or MSA)
- At least 5 years of symptoms
- A clear, strong response to levodopa-your motor score on the UPDRS-III must improve by more than 30% after taking your usual dose
- No major cognitive issues-MMSE above 24 or MoCA above 21
- No uncontrolled depression or psychosis
If your tremors vanish after a levodopa dose but return when it wears off, you’re likely a strong candidate. If your main problem is balance, freezing, or speech-symptoms that don’t respond to levodopa-DBS won’t help much. Those axial symptoms only improve by 20-30% with current tech.
And here’s the hard truth: if you’re hoping DBS will fix your memory, mood, or sleep, you’ll be disappointed. It’s designed for motor symptoms. One patient on the Parkinson’s Foundation Forum said, “I thought it would stop the decline. It didn’t. It just made my good days better.” That’s the reality.
STN vs. GPi: Which Target Is Right for You?
The two most common brain targets for DBS are the subthalamic nucleus (STN) and the globus pallidus interna (GPi). Both improve movement, but they have different trade-offs.
STN stimulation gives you the biggest drop in medication use-often 40-50% less levodopa. That means fewer nausea, hallucinations, and daytime sleepiness from pills. But it can also make some people more prone to mood changes, word-finding trouble, or impulsivity. One Reddit user wrote: “My tremors are gone, but now I forget words mid-sentence. It took speech therapy to fix it.”
GPi doesn’t reduce meds as much, but it’s better at taming dyskinesias. If your biggest problem is uncontrollable twisting movements after taking levodopa, GPi may be the safer pick. The VA/NINDS CSP #468 trial showed GPi reduced dyskinesias by 70% versus 46% with STN. It also tends to have fewer cognitive side effects.
There’s no universal “best” target. It depends on your symptoms, your age, your meds, and your brain. A good team will run you through simulations and discuss your priorities: Do you want fewer pills? Or fewer dyskinesias? Do you work a job that demands sharp focus? Then GPi might be better. Are you mostly bothered by freezing and stiffness? STN could be your best bet.
The Surgery: What Happens on the Day
DBS surgery isn’t done under full anesthesia. You’re awake-partly. You get local numbing and light sedation so you’re calm but responsive. Why? Because the surgeons need you to move, speak, and react while they place the electrodes.
The procedure takes 3 to 6 hours. First, a metal frame is attached to your skull. Then, a high-resolution 3T MRI maps your brain. Using that map, the team drills two small holes (each about the size of a pencil tip) and inserts thin wires (1.27mm wide) into the target area. Microelectrode recording listens to individual brain cells. If you move your hand when they stimulate the right spot, they know they’re on target.
The wires connect to a pacemaker-like device implanted under your collarbone or abdomen. That’s the IPG-implantable pulse generator. It’s about the size of a stopwatch. You’ll go home in a few days. The stimulation doesn’t turn on right away. It takes 2 to 6 weeks for swelling to settle. Then comes the real work: programming.
Programming and Long-Term Management
Getting DBS settings right is like tuning a radio. Too little signal? Symptoms return. Too much? You get muscle tightness, speech slurring, or tingling. It takes months to get it right.
Most patients need 6 to 12 visits over the first year. Each session lasts 30 to 90 minutes. You’ll be asked to keep a symptom diary: when you feel stiff, when meds wear off, when you have dyskinesias. Your neurologist adjusts voltage, frequency, and pulse width. Newer devices let you tweak settings at home via an app, but only after training.
Batteries last 3 to 15 years, depending on the device and usage. Rechargeable models (like Percept™ PC) can last up to 15 years. Non-rechargeable ones need replacement every 3 to 5 years-another small surgery. Hardware problems happen in 5-15% of cases: wires break, leads shift, infections develop. Most are fixable, but they’re stressful.
Long-term results are strong. A 2019 study in Neurology found 85% of patients still had good motor control 10 years after surgery. But DBS doesn’t stop aging. Balance, freezing, and speech issues often get worse over time, no matter how well the device works.
Cost, Access, and Why So Few People Get It
In the U.S., DBS costs between $50,000 and $100,000. Medicare and most insurers cover it if you meet criteria. But getting approval can take 3 to 6 months. You’ll need proof you’ve tried and failed on multiple meds.
Only 15,000 to 20,000 procedures are done each year worldwide. That’s a tiny fraction of the 10 million people with Parkinson’s. Why? Because many neurologists don’t know when to refer. Patients assume it’s a last-resort option. It’s not. The EARLYSTIM trial showed patients who had DBS after 4 years of symptoms did better than those who waited 10 years. Earlier is often better-if you’re a good candidate.
Center volume matters too. Hospitals doing more than 50 DBS cases a year have 20% fewer complications. Look for a center with a dedicated movement disorders team: a neurologist who specializes in PD, a neurosurgeon who does DBS daily, and a neuropsychologist who checks cognition.

Real Stories: What Patients Say
One man in his early 60s, who used to need help getting out of his chair, told his neurologist after STN DBS: “I made my own coffee this morning. For the first time in five years.”
Another woman, a retired teacher, said her dyskinesias were so bad she couldn’t hold a book. After GPi DBS, she started reading to her grandchildren again.
But not all stories are smooth. A man in his 50s developed apathy after STN DBS. He stopped gardening, stopped talking. His wife said, “He’s physically better, but emotionally gone.” That’s why neuropsych testing before surgery is non-negotiable.
And then there’s the myth that DBS makes you “normal.” It doesn’t. You’ll still have Parkinson’s. You’ll still need meds. You’ll still have bad days. But you’ll have more good ones. And for many, that’s enough.
The Future: Closed-Loop, Genetics, and Earlier Intervention
DBS isn’t standing still. The latest systems use “closed-loop” technology-like a thermostat that turns on only when needed. Medtronic’s Percept™ PC records brain signals and adjusts stimulation automatically. Early results show 27% better symptom control than traditional DBS.
Researchers are now looking at genetic markers. People with LRRK2 gene mutations respond 15% better to DBS, according to a 2023 Lancet Neurology study. That could mean future screening includes genetic testing.
The EARLYSTIM-2 trial is testing DBS in patients with just 3 years of Parkinson’s. If it works, the window for intervention could widen dramatically.
And soon, your Apple Watch might talk to your DBS device. If it detects a tremor spike during a walk, it could signal your implant to boost stimulation-no manual input needed.
Final Thoughts: Is DBS Right for You?
If you’ve been living with Parkinson’s for 5+ years, your meds are losing their edge, and you still respond well to levodopa-talk to your neurologist about DBS. Don’t wait until you’re wheelchair-bound or can’t swallow pills. Don’t assume you’re too young or too old. Age isn’t the barrier-response to levodopa is.
Get a full evaluation: neurology, neuropsychology, MRI, and a team review. Ask about target options. Ask about center volume. Ask about long-term support. And be honest with yourself: Are you hoping for a miracle? Or are you hoping for more good days?
DBS won’t fix everything. But for the right person, it gives back something precious: control.
Can DBS cure Parkinson’s disease?
No, DBS does not cure Parkinson’s. It doesn’t stop the brain from degenerating. It only treats motor symptoms that respond to levodopa-like tremors, stiffness, slowness, and dyskinesias. It does not improve balance, speech, swallowing, or cognitive decline. Patients still need medication and will continue to experience disease progression over time.
Is DBS safe for older adults?
Age alone doesn’t disqualify someone. People in their 70s and even 80s have had successful DBS if they’re otherwise healthy. The key factors are cognitive status, overall physical health, and levodopa response-not age. A 75-year-old with good memory and strong medication response often does better than a 60-year-old with early dementia and poor levodopa benefit.
How long does it take to see results after DBS surgery?
You won’t feel the full effect right away. Swelling from surgery takes 2 to 6 weeks to go down. Stimulation usually starts after that. It can take 3 to 6 months of programming visits to fine-tune settings. Most patients notice major improvements within 3 months, but full optimization often takes up to a year.
What are the biggest risks of DBS surgery?
The most serious risk is bleeding in the brain, which happens in 1-3% of cases and can cause stroke-like symptoms. Infection occurs in 3-5% and may require hardware removal. Lead migration or breakage happens in 5-15% over time. Cognitive side effects-like memory lapses or word-finding trouble-are common but often mild and improve with programming adjustments. Not everyone gets these, but they’re real and should be discussed before surgery.
Can DBS help with freezing of gait or balance problems?
Only slightly. Freezing of gait and balance issues are called axial symptoms, and they respond poorly to DBS-typically improving by only 20-30%. These symptoms don’t respond well to levodopa either, which is why DBS isn’t the best solution. Physical therapy, assistive devices, and newer approaches like targeted gait training are more helpful for these issues.
Do I need to stop my Parkinson’s meds after DBS?
No, you don’t stop them completely. Most people reduce their dose by 30-50%, especially if they have an STN target. But you still need some medication to manage symptoms DBS doesn’t fully cover, like non-motor symptoms or axial issues. Stopping meds entirely can lead to sudden worsening. Your neurologist will gradually adjust your dose over weeks or months after DBS is activated.
What if I have a pacemaker or other implanted device?
Having a cardiac pacemaker doesn’t automatically disqualify you, but it adds complexity. The two devices can interfere with each other. Your team will need to check compatibility, use special settings, and coordinate with your cardiologist. Some newer DBS systems are designed to be MRI-safe and compatible with modern pacemakers. Always disclose all implants before surgery.
Are there alternatives to DBS for Parkinson’s?
Yes. Focused ultrasound (Exablate Neuro) is FDA-approved for tremor-dominant Parkinson’s and is non-invasive, but it only works on one side of the brain and doesn’t help with stiffness or slowness. Lesioning surgeries like pallidotomy or thalamotomy are permanent and carry higher risks of permanent side effects. Medication adjustments, physical therapy, and lifestyle changes are always part of the plan. DBS remains the most effective option for advanced motor complications.





Miriam Lohrum
It's funny how we call it a 'pacemaker for the brain' like that makes it sound gentle. But it's really more like hijacking your neural wiring with a tiny, persistent hum. You're not curing anything-you're just hacking the noise. And somehow, that's enough.
archana das
In India, we don't even talk about this. My uncle had Parkinson's for 12 years, and no one ever said DBS was an option. We just prayed, gave him herbs, and waited. It's not just about money-it's about silence. We don't ask for high-tech fixes. We just endure.
Emma Dovener
I work with movement disorder patients daily. The biggest mistake I see is waiting until they're practically bedridden. If someone still responds to levodopa, even if it's fading, they're a candidate. Early referral saves years of decline. Don't wait for the worst day to ask for help.
Asha Jijen
So you spend 100k to get back the ability to button your shirt? And then you get weird mood swings and forget your kid's name? Sounds like a fair trade if you ask me. At least the pills made me sleepy, not emotionally hollow
Edward Batchelder
I want to emphasize, with all due care and precision, that DBS is not a miracle, nor is it a last resort-it is, in fact, a powerful, evidence-based intervention that should be considered earlier than most patients are led to believe. Many clinicians still operate under outdated assumptions, and that is a systemic failure we must correct.
reshmi mahi
USA spending 100k on brain pacemakers while my cousin can't afford insulin? 🤡 We live in a world where your dignity costs more than a used Tesla. But hey, at least you can wave to your grandkids again. #FirstWorldProblems
laura lauraa
I find it deeply troubling that the medical community continues to promote this invasive, high-risk, financially exploitative procedure as if it were a benign solution. The emotional toll on families-particularly when apathy sets in-is rarely acknowledged in these glossy success stories. Are we really so desperate for control that we will trade humanity for motor function?
Gayle Jenkins
If you're reading this and wondering if DBS is right for you-ask your neurologist this: 'If this were your parent, would you wait until they couldn't stand up?' Don't let fear or misinformation delay your evaluation. This isn't about being brave-it's about being informed. You deserve more than just surviving. You deserve better days.