Diabetes Food Carb Calculator
How It Works
Calculate net carbs (total carbs minus fiber) for your meals. This helps you stay within your daily carb limit while managing blood sugar effectively.
Our sample meal plan (shown below) targets 130g net carbs per day - a common goal for many adults with type 2 diabetes.
Daily Carb Goal
Daily Target: 130g net carbs
Your Meal Plan
No foods added yet. Select a food and portion to begin.
Tip: Combine high-fiber foods with protein for better blood sugar control.
Living with type 2 diabetes means you need to watch what you eat, but it doesn’t have to feel like a punishment. The right foods can steady your blood sugar, boost insulin sensitivity, and even keep cravings at bay. Below is a straight‑forward list of ten powerhouse foods that fit easily into everyday meals.
Why Food Choices Matter for Type 2 Diabetes
When you have Type 2 Diabetes is a chronic condition where the body either resists insulin or doesn’t produce enough, leading to elevated blood glucose levels. Small spikes after meals can wear down blood vessels over time, raising the risk of heart disease, kidney trouble, and vision loss. Managing carbs, fiber, and healthy fats is the cornerstone of keeping those spikes low. Studies from the American Diabetes Association show that diets rich in fiber and low‑glycemic carbs reduce A1C by up to 0.5% in just three months.
1. Blueberries - Tiny Berries, Big Impact
Blueberries are low‑glycemic fruits packed with anthocyanins, antioxidants that improve insulin signaling. One cup (150 g) provides about 4 g of fiber and only 15 g of carbs, making them perfect for a snack or a smoothie base. Toss them into Greek yogurt for a protein‑rich breakfast that steadies glucose for hours.
2. Leafy Greens - The Low‑Calorie Backbone
Leafy Greens such as spinach, kale, and Swiss chard are virtually carb‑free and loaded with magnesium, a mineral linked to better insulin action. A cup of cooked kale offers only 7 g of carbs but 3 g of fiber and plenty of vitamin K. Use them as a base for salads, stir‑fries, or blended soups to bulk up meals without spiking sugar.
3. Oats - Slow‑Release Carbohydrate
Oats are a whole grain that supplies beta‑glucan, a soluble fiber that slows carbohydrate absorption. A half‑cup of rolled oats (40 g) supplies 27 g of carbs, but 4 g of that is fiber, giving a net carb count of 23 g. Pair oats with cinnamon and a handful of nuts for a breakfast that tackles cravings early.
4. Almonds - Crunchy Healthy Fat
Almonds deliver monounsaturated fats, protein, and 3.5 g of fiber per 28‑g serving. The combination reduces post‑meal glucose peaks by as much as 20% in clinical trials. Keep a small container at work for an easy, satiating snack.

5. Legumes - Plant‑Based Protein Powerhouses
Legumes (lentils, chickpeas, black beans) provide about 15 g of protein and 8 g of fiber per half‑cup cooked. Their low glycemic index (GI ≈ 30) means blood sugar rises gradually. Add them to salads, soups, or as a meat substitute in tacos.
6. Fatty Fish - Omega‑3 Boost
Fatty Fish such as salmon, mackerel, and sardines supply EPA/DHA omega‑3s that reduce inflammation and improve insulin sensitivity. A 100‑g serving provides 22 g of protein and virtually no carbs. Grill with lemon and herbs for a heart‑healthy dinner.
7. Avocado - Creamy Fiber and Healthy Fat
Avocado offers 7 g of fiber and 15 g of monounsaturated fat per half fruit, helping slow carbohydrate digestion. Its creamy texture works well in salads, smoothies, or as a spread instead of butter.
8. Greek Yogurt - Protein‑Rich Dairy
Choose plain, low‑fat Greek yogurt (about 10 g of protein and 6 g of carbs per 150 g). The high protein content promotes satiety, while probiotics support gut health, which recent research links to better glucose regulation.
9. Cinnamon - Spice with a Sweet Effect
Adding 1‑2 teaspoons of cinnamon to oatmeal, coffee, or baked goods can lower fasting blood glucose by up to 0.2% in some studies. The compound cinnamaldehyde appears to enhance insulin receptor activity.
10. Sweet Potatoes - Nutritious Starchy Alternative
Sweet potatoes have a lower GI (≈ 44) than regular potatoes and contain 3 g of fiber per 100 g. Roast them with olive oil and rosemary for a flavorful side that won’t crash your sugar levels.
How to Combine These Foods into a Daily Plan
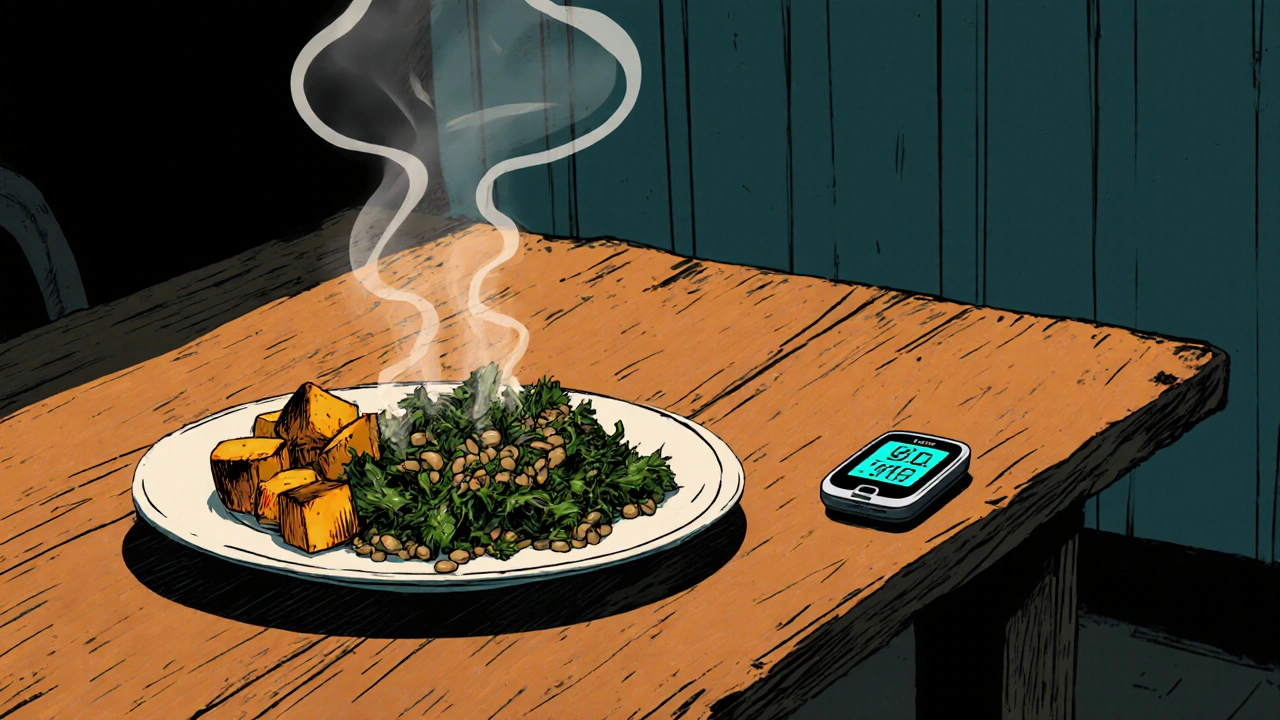
Below is a sample day that hits all food groups while keeping total net carbs around 130 g - a typical target for many adult diabetics.
| Meal | Food | Portion | Net Carbs |
|---|---|---|---|
| Breakfast | Oatmeal with blueberries, cinnamon, and almonds | ½ cup oats, ½ cup blueberries, 1 tsp cinnamon, 10 g almonds | 28 g |
| Snack | Greek yogurt | 150 g | 6 g |
| Lunch | Spinach salad with grilled salmon, avocado, chickpeas | 2 cups spinach, 100 g salmon, ½ avocado, ¼ cup chickpeas | 12 g |
| Snack | Blueberries | ¾ cup | 13 g |
| Dinner | Stir‑fried kale with lentils and a side of roasted sweet potato | 1 cup kale, ½ cup lentils, ½ cup sweet potato | 31 g |
| Evening snack (optional) | Almonds | 15 g | 2 g |
Notice the balance of fiber, protein, and healthy fats at each eating window. Pair meals with a glass of water or unsweetened tea to stay hydrated and avoid sugary drinks.
Practical Tips to Maximize Benefits
- Portion control: Even low‑GI foods can raise glucose if you eat too much. Use a food scale or the hand‑portion method (a palm of protein, a fist of vegetables, a cupped hand of carbs).
- Cook with healthy fats: Olive oil, avocado oil, or a small pat of butter keep the taste while slowing carb absorption.
- Snack wisely: Choose protein‑rich or fiber‑rich snacks (nuts, Greek yogurt, a small fruit) over candy or chips.
- Stay consistent: Eating at similar times each day helps your body predict insulin needs.
- Monitor response: Use a continuous glucose monitor (CGM) or finger‑stick tests to see which foods keep you in target range (70‑130 mg/dL fasting).
Common Pitfalls and How to Avoid Them
Even the best food list can backfire if you slip into these habits:
- Relying on “diabetic‑safe” labels: Many packaged snacks boast the term but still contain hidden sugars or refined carbs. Always read the nutrition facts.
- Skipping meals: Skipping breakfast often leads to overeating later, causing larger glucose swings.
- Over‑seasoning with sugary sauces: Barbecue, ketchup, and teriyaki sauces can add 5‑10 g of sugar per tablespoon. Opt for herb‑based marinades.
- Neglecting fiber: Fiber slows glucose absorption. If a meal feels low‑fiber, add a side of beans or a sprinkle of chia seeds.
Frequently Asked Questions
Can I eat fruit if I have type 2 diabetes?
Yes, but choose low‑glycemic options like berries, cherries, or a small apple. Pair fruit with protein or fat (e.g., Greek yogurt) to blunt the sugar rise.
How many servings of vegetables should I aim for each day?
Aim for at least five 1‑cup servings of non‑starchy vegetables (leafy greens, broccoli, peppers) daily. This provides fiber and micronutrients that aid glucose control.
Is it okay to eat whole‑grain bread?
Whole‑grain bread is better than white bread because it has more fiber and a lower GI, but watch portion size. Two slices (≈ 30 g) usually fit into a balanced meal.
Do artificial sweeteners affect blood sugar?
Most non‑nutritive sweeteners (stevia, erythritol) have little to no impact on glucose, but some people experience gut‑microbiome changes. Test your response and use them sparingly.
How often should I check my blood sugar after meals?
A good rule is to test 1-2 hours after starting a meal. This timing captures the peak glucose response for most people.
Integrating these ten foods into your everyday menu isn’t a diet-it’s a lifestyle tweak that can keep your blood sugar steady and your taste buds happy. Start with one or two additions this week, track how you feel, and build from there. Your future self will thank you.





Nhasala Joshi
It’s not a coincidence that the “top 10” list conveniently omits any mention of the ultra‑processed snack empire that’s secretly funding some of these “healthy” campaigns 😈📈. The hidden agenda is clear: keep us hypnotized with berry‑filled smoothies while the sugar conglomerates tout their “low‑glycemic” miracle powders. Remember, every time you sprinkle cinnamon, a boardroom decides whether to green‑light another line of artificial sweeteners. The food lab‑coat elite are mixing meta‑data with our meals, turning dietary guidelines into a covert neuromarketing experiment. Stay vigilant, question the source, and don’t let the glittering berries blind you to the larger manipulation 🚨.
Brian Van Horne
Your compilation offers a clear, well‑structured overview of glycemic management options.
Emma Williams
I appreciate the practical tone of the guide and the balanced meal plan examples. It’s helpful to see specific portions and net carb counts for each meal. Adding a note about how to adjust the plan for lower activity days could make it even more flexible. Overall the content is user‑friendly and actionable.
Stephanie Zaragoza
While the article admirably lists nutrient‑dense foods, it neglects to address the glycemic variability inherent in individual metabolic phenotypes, which is a glaring oversight; consequently, readers may overestimate the uniformity of the suggested net‑carb targets. Moreover, the reliance on generic serving sizes fails to consider cultural dietary patterns, an omission that could undermine the plan’s global applicability. The omission of low‑fat dairy alternatives, despite evidence supporting their role in satiety, further diminishes the guide’s comprehensiveness. A more nuanced discussion of insulin resistance stages, coupled with a stratified carbohydrate algorithm, would elevate the recommendation from merely adequate to exemplary.
James Mali
In the grand tapestry of nutrition, this list is a modest stitch-adequate but unremarkable. It serves its purpose, though it could benefit from a dash more culinary imagination. 🤔
Tracy O'Keeffe
Ah, the saccharine allure of a “Top 10” list, a siren song that lulls the masses into complacency whilst the culinary aristocracy continues its clandestine ballet of flavor manipulation. I must protest, not out of sheer contrarian impulse, but because the very premise that ten foods can singularly “control” a multifaceted metabolic disorder is a reductionist myth perpetuated by industry‑sponsored pundits.
First, the glorification of blueberries as a panacea ignores the longitudinal data that demonstrates mere modest reductions in postprandial spikes, a nuance lost amidst the glossy stock images.
Second, the reverence for leafy greens, though nutritionally sound, betrays an elitist bias toward produce that demands temperate climate imports, rendering the advice impractical for subsistence farmers in arid regions.
Third, the oat ode fails to acknowledge the gluten‑sensitive cohort whose intestinal permeability spikes under beta‑glucan exposure, a fact buried beneath the oat‑centric optimism.
Fourth, almonds are praised for monounsaturated fats, yet the environmental toll of almond orchards-water scarcity, monoculture pesticide runoff-is conveniently omitted, a silent concession to agribusiness propaganda.
Fifth, legumes are heralded without mention of phytate content, which can inhibit mineral absorption unless properly fermented-a culinary alchemy absent from the guide’s simplicity.
Sixth, the salmon laudation glosses over the pervasive issue of mercury bioaccumulation, a toxin that subtly undermines endocrine function while the article basks in omega‑3 rhetoric.
Seventh, the avocado encomium overlooks the socio‑economic chasm it creates, where affluent markets hoard a fruit that could otherwise ameliorate micronutrient deficiencies in impoverished diets.
Eighth, Greek yogurt is championed, yet the fermentative cultures vary wildly, and not all strains confer the purported probiotic benefits, a scientific caveat omitted for brevity.
Ninth, cinnamon’s sweet whisper is intoxicating, but the text sidesteps the potential hepatotoxicity of coumarin in Cassia cinnamon, a risk factor for liver health.
Tenth, sweet potatoes are praised, yet their glycemic index can skyrocket if over‑roasted, a culinary hazard unaddressed.
Beyond the list, the suggested meal plan, while aesthetically balanced, presumes access to a calibrated food scale and a repertoire of culinary skills that the average diabetic consumer simply does not possess.
The narrative also neglects the psychosocial dimension of eating-cultural identity, emotional eating patterns, and socioeconomic constraints-that are critical determinants of long‑term adherence.
Moreover, the nutriton analysis omitted critical micronutrient interactions, a glaring omission.
In sum, while the article offers a veneer of practicality, it is a palatable confection that masks deeper complexities, and those seeking true metabolic sovereignty would be well advised to interrogate each recommendation with a skeptical mind. 🍽️
Natala Storczyk
Patriotic readers, heed this: our nation's farmers have cultivated kale, oats, and beans long before any foreign corporation could dictate dietary trends!!! The USDA’s guidelines, rooted in American soil, champion these very foods as the backbone of our health!!! Let us reject imported “miracle” diets and embrace home‑grown nutrition for the sake of national strength!!!
nitish sharma
It is commendable to celebrate indigenous produce, and I encourage you to integrate these recommendations with balanced portions and regular monitoring. By harmonizing traditional staples with evidence‑based guidelines, individuals can achieve sustainable glycemic control while honoring cultural heritage. I remain at your service for any further clarification.