Anticoagulant Basics: How Blood Thinners Work and What You Need to Know
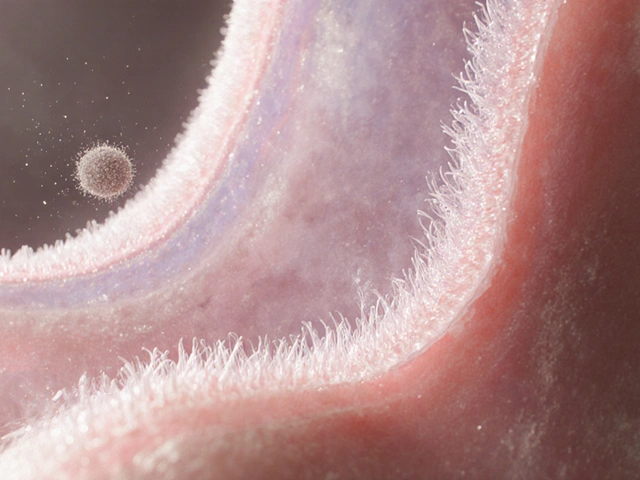
Anticoagulants are medicines that keep your blood from clotting too much. They’re often called blood thinners, even though they don’t actually thin the blood. The goal is to stop dangerous clots that can cause strokes, heart attacks, or block blood flow in the legs.
If you’ve been told to take an anticoagulant, it’s usually because you have a condition like atrial fibrillation, a recent deep‑vein thrombosis, or you’re recovering from heart valve surgery. The drug works by interfering with the clotting process, either by blocking certain proteins or by stopping platelets from sticking together.
Common Anticoagulant Types
There are two main families of blood thinners. The older group includes warfarin (Coumadin) and a few others that need regular blood tests. Warfarin works by lowering vitamin K levels, which are needed for clot formation. Because diet and other meds can change how warfarin acts, you’ll need frequent INR checks to stay in the right range.
The newer group is called direct oral anticoagulants or DOACs. This includes dabigatran (Pradaxa), rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Savaysa). DOACs target specific clotting factors and generally don’t require routine blood monitoring. They’re taken once or twice a day, and food interactions are minimal compared with warfarin.
Safety and Monitoring
Bleeding is the biggest risk with any anticoagulant. Minor bruises or nosebleeds can happen, but serious bleeding in the brain or gut is rare if you follow the doctor’s instructions. If you notice unusual bleeding, black stools, or a sudden headache, call your health provider right away.
Always tell every doctor, dentist, and pharmacist that you’re on an anticoagulant before any procedure. Minor dental work or a small cut usually doesn’t need to stop the medication, but bigger surgeries might require a short pause under medical supervision.
Alcohol, certain herbs (like ginkgo or high‑dose garlic), and many over‑the‑counter pain relievers can increase bleeding risk. Stick to acetaminophen for pain if you need it, and avoid ibuprofen or naproxen unless your doctor says it’s safe.
Storing your medication properly matters too. Keep pills in a cool, dry place and out of reach of children. If you miss a dose, check the label—most DOACs say to take it as soon as you remember, but don’t double up. For warfarin, take the missed dose at your usual time and resume the regular schedule.
Traveling? Pack enough pills to last the trip plus a few extras, and keep them in your carry‑on bag in case your luggage gets lost. Bring a copy of your prescription and a brief note about why you’re taking the anticoagulant.
Finally, know your signs of a clot forming while on therapy. Sudden leg swelling, pain, or redness could mean a new clot despite the medication. If that happens, get medical help fast—early treatment works best.
Understanding how anticoagulants work, the differences between warfarin and DOACs, and the steps to stay safe can make the treatment feel less scary. Keep open communication with your health team, follow dosing rules, and you’ll lower your risk of dangerous clots while minimizing side effects.