What Happens When Mast Cells Go Rogue
Mast cells are your body’s first line of defense at the borders-skin, lungs, gut, and nasal passages. They’re not meant to cause trouble. But when they activate too easily or too often, they dump out a storm of chemicals that make you feel awful. This isn’t just allergies. It’s chronic fatigue, brain fog, hives, stomach cramps, dizziness, and even fainting. This is mast cell activation syndrome, or MCAS, and it’s more common than most doctors realize.
Think of mast cells like tiny alarm clocks packed with chemicals. When triggered, they explode open in seconds. Histamine rushes out first-that’s the stuff that makes your nose run, your skin itch, and your throat swell. Then come tryptase and chymase, enzymes that tear at tissues. Within minutes, prostaglandin D2 and leukotriene C4 flood in, tightening airways and spiking inflammation. Hours later, cytokines like TNF-alpha keep the fire going, turning a quick reaction into days of misery.
What sets off these explosions? It’s not always pollen or peanuts. For many, it’s heat, stress, NSAIDs like ibuprofen, alcohol, or even a hot shower. A 2022 survey of over 1,200 MCAS patients found that 68% react to NSAIDs, 63% to alcohol, and 52% to emotional stress. These aren’t random triggers-they’re signals that the mast cells have become hypersensitive.
The Chemical Storm: What Gets Released and When
Mast cells don’t just spray everything at once. They release their weapons in waves, and knowing the order helps explain why symptoms change over time.
Within 15 to 90 seconds of activation, pre-formed mediators burst out. Histamine makes up 10-15% of the granule’s dry weight. Tryptase, which doctors test for in blood, accounts for 20-30% of the granule’s protein. These are stored tightly in granules, held in place by negatively charged sugars called heparin and chondroitin sulfate. If those sugars lose their charge-due to genetic changes or inflammation-the granules leak, even without a trigger.
Then, within minutes, the cell starts making new stuff. Prostaglandin D2, derived from fatty acids, causes flushing and low blood pressure. Leukotriene C4 is a powerful bronchoconstrictor-this is why asthma flares so fast in MCAS. Platelet-activating factor (PAF) can trigger shock. These aren’t just side effects; they’re direct results of mast cell signaling gone wrong.
Hours later, cytokines like IL-6 and IL-13 start pouring out. These don’t cause immediate symptoms, but they keep the immune system on high alert. That’s why some people feel exhausted for days after a single trigger. The body isn’t just reacting-it’s stuck in a loop.
How Mast Cell Stabilizers Work-And Why They’re Not Magic
Mast cell stabilizers like cromolyn sodium and ketotifen don’t block histamine. They don’t calm inflammation. They stop the explosion before it happens.
Cromolyn sodium, approved in the U.S. in 1973, works by plugging the calcium channels mast cells need to open their granules. No calcium influx? No degranulation. It’s like putting a lock on the alarm system. But it only works if you take it before exposure. If you wait until you’re breaking out in hives, it’s too late.
Studies show cromolyn reaches peak levels in the blood 2-4 hours after taking it, but it’s cleared quickly-half gone in 1.5 hours. That’s why patients take it four times a day. Doses start at 100 mg per dose and often climb to 200-400 mg four times daily. The goal isn’t to feel perfect-it’s to reduce the frequency and severity of attacks.
Ketotifen, another stabilizer, does the same job but also has mild antihistamine effects. In a 2018 study, it cut MCAS symptoms by 50-70% at doses of 1-4 mg twice daily. But neither drug stops cytokine production. That’s the big limitation. You can block histamine and tryptase, but the slow-burning cytokine fire still rages.

Why Many People Struggle With Stabilizers
Stabilizers sound simple. But in practice, they’re messy.
First, they take time. One patient on MastAttack.org reported her anaphylactic episodes dropped by 70% after eight weeks on cromolyn. That’s not a quick fix. Most people give up before the 4-6 week mark.
Second, side effects are real. A 2021 Drug Safety study found 35% of cromolyn users had nausea or diarrhea. Fifteen percent quit because of it. The liquid form tastes awful-patients rated it 2.1 out of 5 in a 2019 survey. Some kids need feeding tubes just to get it down.
Third, it doesn’t work for everyone. A 2022 survey of MCAS patients showed 87% saw *some* improvement with stabilizers, but only 43% got full control. That means more than half still have daily symptoms. For them, stabilizers are a tool-not a cure.
Compare that to biologics like omalizumab, which targets IgE. Those work for 70-80% of patients, but they cost thousands per month and require injections. Stabilizers are cheap, oral, and safe for long-term use. They’re the baseline, not the finish line.
Diagnosis: The Long Road to Getting Help
Most MCAS patients see six to ten doctors over three to five years before getting a real diagnosis. Many are told they have anxiety, IBS, or chronic fatigue syndrome. That’s because the symptoms are all over the map-skin, gut, brain, heart, lungs. There’s no single test.
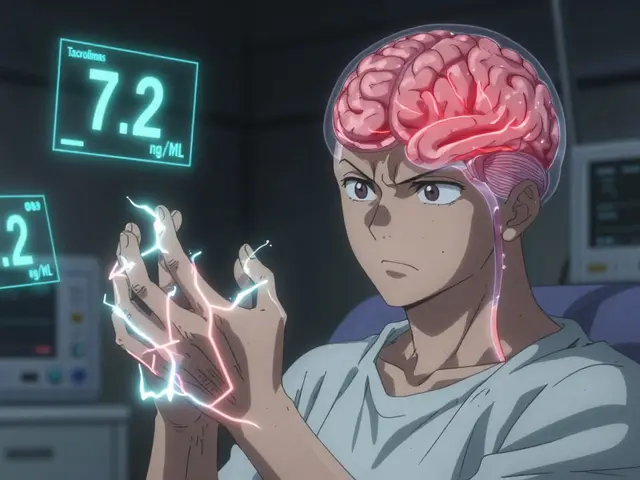
Doctors look for three things: symptoms matching MCAS, improvement with mast cell-targeted meds, and elevated biomarkers. The gold-standard test is serum tryptase. A rise of more than 20% plus 2 ng/mL above baseline is considered diagnostic under the ICON-MCD guidelines. But not everyone with MCAS has elevated tryptase. The American Academy of Allergy, Asthma & Immunology says clinical diagnosis is enough if the rest fits.
Urinary tests for methylhistamine and N-methyl-β-hexosaminidase are also used. Successful treatment means a 30% drop in these markers over time. But testing isn’t always available. Many labs don’t offer it. And even if they do, results take weeks.
Genetic testing is becoming more common. About 30% of MCAS patients have mutations in genes like KIT, TPSAB1, or CBL-genes that control how mast cells grow and respond. These aren’t inherited diseases like cystic fibrosis. They’re somatic mutations, meaning they happen in the body over time, often after trauma or chronic inflammation.

What’s Next: The Future of MCAS Treatment
The field is changing fast. In 2023, the FDA approved avapritinib for advanced systemic mastocytosis. It targets the KIT D816V mutation, which drives abnormal mast cell growth. In trials, it cut mediator levels by 60% at 200 mg daily.
But avapritinib is for severe cases. For most MCAS patients, the next wave of drugs is more promising. SYK kinase inhibitors-currently in Phase II trials-are showing 75% reduction in mediator release at 100 mg daily. These drugs block signals inside the mast cell before they can trigger release. Unlike stabilizers, they might work even after a trigger has started.
Other targets include KIT D816V blockers, mast cell-specific monoclonal antibodies, and drugs that reset the mast cell’s sensitivity. The goal isn’t just to stop reactions-it’s to make mast cells behave normally again.
By 2030, experts predict next-gen therapies could control symptoms in 80-90% of MCAS patients. But until then, stabilizers remain the most accessible, affordable, and safe option for millions.
Living with MCAS: Practical Steps That Actually Help
If you’re managing MCAS, here’s what works:
- Start low, go slow with cromolyn. Begin at 100 mg four times a day. Wait four weeks before increasing. Don’t rush.
- Track triggers. Use the mast cell trigger wheel-NSAIDs, alcohol, heat, stress, foods. Write down what you ate, where you were, how you felt. Patterns emerge.
- Test your markers. Ask for urinary methylhistamine and N-methyl-β-hexosaminidase before and after treatment. Numbers matter more than how you feel.
- Find a specialist. The Mast Cell Disease Society lists 350 verified doctors in the U.S. and Europe. Don’t waste time with providers who don’t know MCAS.
- Be patient. Improvement takes months. Some people feel worse at first as their body adjusts. That’s normal.
MCAS isn’t a death sentence. It’s a complex condition that’s finally being understood. Stabilizers won’t fix everything-but they give you back control. And in a world where your own body feels like the enemy, that’s everything.
Can mast cell stabilizers cure MCAS?
No, mast cell stabilizers don’t cure MCAS. They prevent mast cells from releasing mediators, which reduces symptoms. But they don’t fix the underlying hypersensitivity or genetic changes. They’re a management tool, not a cure.
How long does it take for cromolyn sodium to work?
Most people need 4 to 8 weeks to see noticeable improvement. Some report changes after 2 weeks, but full effects often take longer. Patience is key-stopping too early means missing the benefit.
Are mast cell stabilizers safe for long-term use?
Yes. Cromolyn sodium and ketotifen have been used safely for decades. Side effects like nausea or diarrhea are usually mild and improve over time. Unlike steroids or immunosuppressants, they don’t weaken the immune system.
Why do some people with MCAS react to alcohol?
Alcohol triggers mast cells directly and also blocks the enzyme that breaks down histamine (DAO). This double hit causes histamine to build up rapidly. Even small amounts can cause flushing, headaches, or nausea in MCAS patients.
Is MCAS the same as histamine intolerance?
No. Histamine intolerance means your body can’t break down histamine from food. MCAS means your mast cells are releasing too much histamine and other mediators. You can have both, but they’re different conditions. MCAS requires different treatment.
Can stress really trigger mast cell activation?
Yes. Stress releases substance P and cortisol, both of which directly activate mast cells. Emotional stress isn’t "all in your head"-it’s a biological trigger. Many patients report flares after arguments, job loss, or even sleep deprivation.




Frank Declemij
Mast cell stabilizers aren't magic but they're the only thing keeping me functional. Took me 6 months to find the right dose but now I can shower without collapsing. Cromolyn's a pain to take but it's cheaper than ER visits.
Pawan Kumar
One must question the pharmaceutical-industrial complex's deliberate obfuscation of mast cell pathophysiology. The FDA's approval of avapritinib, while ostensibly progressive, merely reinforces the reductionist paradigm that ignores epigenetic dysregulation as the true root cause. Are we treating cells-or are we appeasing patent holders?
Keith Oliver
Bro, cromolyn tastes like burnt plastic and your gut hates you for it. I took it for 3 weeks, threw up twice a day, and still got hives. Then I tried ketotifen-same crap, but now I'm sleepy too. Why is nothing easy? Someone get us a pill that doesn't suck.
Robin Keith
It’s not merely the mast cells that are malfunctioning-it’s the entire ontological framework of modern immunology that has failed us. We’ve reduced the body to a series of biochemical pathways, as if the soul were irrelevant, as if the trauma stored in the fascia, the grief held in the gut, the unspoken rage that vibrates through the autonomic nervous system… none of it matters. And so we give people pills that plug calcium channels while ignoring the fact that their mother never hugged them, that their workplace is a warzone of microaggressions, that their body is screaming because it has been abandoned by a culture that confuses efficiency with healing.
Stabilizers? They’re bandaids on a hemorrhage. The real cure is radical self-acceptance, ancestral healing, and a return to circadian rhythm-aligned living. But no, let’s just keep prescribing cromolyn and calling it medicine.
And yet-I still take it. Because even a broken system is better than no system at all.
Sheryl Dhlamini
I cried when I finally got diagnosed. After 7 years of being told I was ‘just anxious’-I had a name for the storm inside me. Stabilizers don’t fix everything, but they gave me back my life. Not perfect. Not easy. But mine.
Laia Freeman
OMG YES. I started cromolyn and thought I was gonna die from the nausea. But after 3 weeks? My brain fog lifted. I could finally read a book without falling asleep. I still take it 4x a day and I hate the taste but I’m not giving up. You gotta be stubborn with this stuff 💪
rajaneesh s rajan
So we’re treating symptoms with drugs while ignoring that 90% of us got this after a bad breakup, a toxic job, or a viral infection nobody took seriously. We’re putting locks on alarm clocks while the house is on fire. The real fix? Stop living like a machine. Sleep. Breathe. Say no. But hey, take your cromolyn. It’s cheaper than therapy.
paul walker
Just started ketotifen last week. Still getting dizzy but my hives are down 80%. I’m not giving up. If you’re reading this and you’re on the fence-just hang in there. It gets better. I promise.
Andy Steenberge
For anyone new to MCAS: don’t compare your journey to someone else’s. My friend got relief in 2 weeks. I took 11. Both of us are fine now. It’s not about speed-it’s about consistency. And yes, the taste sucks. But so does being bedridden. Pick your poison.
Alex Flores Gomez
Stabilizers are just bandaids. Real fix? Avoid all triggers. No alcohol. No stress. No heat. No NSAIDs. No carbs. No life. Oh wait-then what’s the point? We’re all just waiting for the next miracle drug that’ll come with a $10k price tag and a 2-year waitlist.