Low-dose CT is a specialized imaging test that uses low radiation to scan lungs. It's the only screening method proven to save lives in high-risk smokers by finding cancer early.
Why Lung Cancer Screening Matters
Lung cancer kills more people than breast, prostate, and colorectal cancers combined. In 2020, it caused over 135,000 deaths in the U.S. alone. The good news? Finding lung cancer at stage 1 gives an 80% chance of survival. By stage 4, that drops to just 6%. Low-dose CT screening finds tumors before symptoms appear, making treatment far more effective.
Who Qualifies for Screening?
The U.S. Preventive Services Task Force (USPSTF) updated guidelines in 2021 to include more people. You qualify if you:
- Are between 50 and 80 years old
- Have smoked at least 20 pack-years (e.g., one pack daily for 20 years, or two packs daily for 10 years)
- Currently smoke or quit within the past 15 years
Before 2021, screening was limited to those 55-80 with 30 pack-years. This change added 14.5 million more Americans eligible for screening. Medicare covers annual scans for ages 50-77 with the same smoking history requirements.
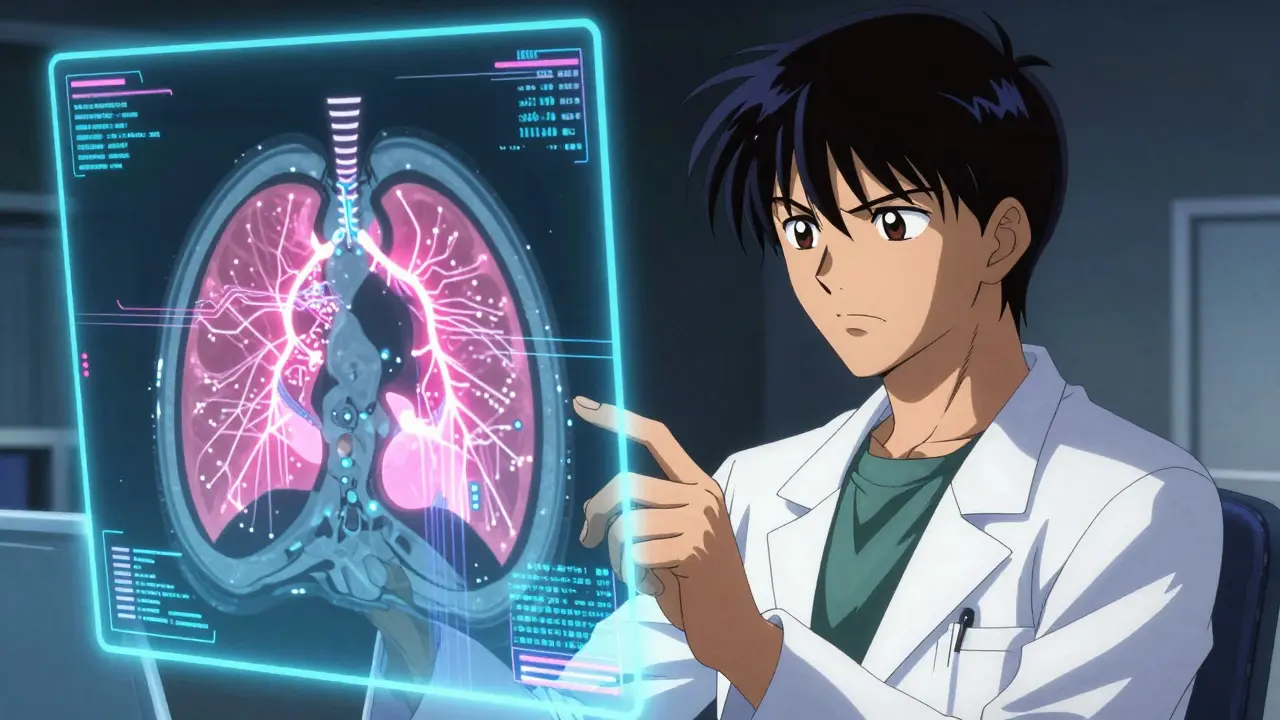
How Low-Dose CT Works
During the scan, you lie on a table while an X-ray machine rotates around you. It takes less than 10 minutes and uses only 1.5 millisieverts of radiation-about one-third of a standard CT scan. No needles or special prep are needed. The machine creates detailed 3D images of your lungs, showing tiny abnormalities doctors might miss with regular X-rays.
| Criteria | 2013 Guidelines | 2021 Update |
|---|---|---|
| Age Range | 55-80 | 50-80 |
| Pack-Year Requirement | 30 | 20 |
| Smoking Status | Current or quit within 15 years | Current or quit within 15 years |

Benefits vs. Risks
The landmark National Lung Screening Trial (NLST) in 2011 showed LDCT screening reduced lung cancer deaths by 20% compared to chest X-rays. For every 1,000 people screened annually for 3 years, about 3 lives are saved. However, there are risks:
- False positives: About 13.9% of scans show something suspicious that turns out to be harmless. This can lead to unnecessary biopsies or anxiety.
- Radiation exposure: While low, repeated scans over time add up. The benefit outweighs this risk for high-risk smokers.
- Overdiagnosis: Some slow-growing cancers might never cause harm, but screening detects them anyway.
What Happens After Your Scan?
Results follow the Lung-RADS system (Lung Imaging Reporting and Data System). This standardizes how doctors interpret scans:
- Category 1 (Negative): No nodules found. Repeat scan in 1 year.
- Category 2 (Benign): Small, harmless nodules. Repeat in 1 year.
- Category 3 (Probably Benign): Small nodules that need monitoring. Repeat in 6 months.
- Category 4 (Suspicious): Larger or irregular nodules. Requires further testing like a biopsy.
Only 1.5% of scans show cancer, but catching it early means surgery can often cure it.
Current Challenges
Despite proven benefits, only 8.3% of eligible smokers get screened. Major barriers include:
- Lack of provider recommendations (42% of cases)
- Unawareness of eligibility (29%)
- Transportation issues (19%)
Black Americans are 20% less likely to get screened than White Americans, even with higher lung cancer rates. Rural areas face shortages of ACR-accredited facilities-only 40% of U.S. counties have one. Some patients travel over 100 miles for scans.
What's Next for Screening?
New tools are improving accuracy. In September 2023, the FDA approved the first AI software (LungAssist by VIDA Diagnostics) for LDCT scans. It reduced false positives by 15.2% in trials. Researchers are also refining risk models like PLCOm2012, which uses education level, family history, and symptoms to better identify high-risk individuals. The goal is to expand screening access while minimizing unnecessary procedures.
Frequently Asked Questions
What is a pack-year?
A pack-year measures smoking history. Multiply packs smoked daily by years smoked. For example, one pack a day for 20 years = 20 pack-years. Two packs a day for 10 years = 20 pack-years. This helps doctors assess cancer risk accurately.
How often should I get screened?
Annual scans are recommended for eligible smokers. Stop screening if you've quit smoking for 15+ years, develop serious health issues limiting life expectancy, or reach age 81. Regular follow-ups are crucial-missing a scan could delay cancer detection.
Is LDCT covered by insurance?
Yes. Medicare covers annual scans for ages 50-77 with qualifying smoking history. Most private insurers follow USPSTF guidelines and cover screening without copays under the Affordable Care Act. Always check with your provider before scheduling.
What if my scan shows a nodule?
Most lung nodules are harmless. Your doctor will use Lung-RADS to determine next steps. Small nodules may need a repeat scan in 6-12 months. Larger or irregular ones might require a biopsy or PET scan. Only 1.5% of scans show cancer, and early-stage tumors are often curable with surgery.
Can non-smokers get screened?
No. Current guidelines only cover smokers or recent quitters. Non-smokers have very low lung cancer risk, and screening isn't recommended. However, those with strong family history or radon exposure should discuss personalized options with their doctor.



Pamela Power
Low-dose CT screening is the only thing standing between death and early detection for smokers, yet the current guidelines are laughably outdated. They're still clinging to that 55-80 age range like it's gospel, ignoring the fact that lung cancer doesn't care about arbitrary numbers. I've seen 45-year-olds with stage 4 cancer who were never screened because they didn't meet the arbitrary 20 pack-year threshold. That's pure negligence. The USPSTF update was a tiny step forward but still too conservative. We need to expand eligibility to include anyone with a history of smoking, regardless of age or pack-years. The risk factors are way more nuanced than this one-size-fits-all approach. They're missing so many high-risk individuals. And the barriers to access? Pathetic. Rural areas don't have facilities, and providers don't even mention it. This is a systemic failure that's costing lives. It's not rocket science to fix this, but nobody wants to do the work. We need to prioritize this like it's a national emergency. Stop being complacent and start saving lives. This isn't just about numbers-it's about human lives being thrown away because of bureaucratic inertia.
Bella Cullen
Screening is good but the guidelines are too strict. They should lower the age. There's a racial disparity in screening rates. Black Americans get screened way less. Rural areas lack access. It's all about money. This needs fixing.
anjar maike
This is vital. 👍
Sam Salameh
As an American, I'm proud we're leading in lung cancer screening tech. But we need to do better for all citizens. The USPSTF guidelines are solid, but maybe we can expand them without compromising safety. Let's make sure every American has access, especially in rural areas. This is a national priority. We can do this right.
divya shetty
It is imperative to address the racial disparities in lung cancer screening. The data clearly shows systemic inequities that must be rectified immediately. Additionally, the guidelines should be expanded to include younger individuals with significant smoking histories. The current threshold of 20 pack-years is arbitrary and excludes many at risk. Furthermore, access to screening facilities must be improved nationwide, particularly in underserved communities. This is a moral obligation, not a matter of convenience.
Phoebe Norman
LDCT screening is critical for early detection but false positives remain a significant issue. The NLST data shows a 20% reduction in mortality but the 13.9% false positive rate leads to unnecessary procedures. Lung-RADS categorization helps but we need better AI integration like LungAssist to reduce false positives. The radiation exposure is low but cumulative effects are a concern for frequent screenings. Early stage detection offers 80% survival but late stage is 6%. This is why we need to expand access but also refine the criteria to avoid overdiagnosis. The current system isn't perfect but it's the best we have.
Tehya Wilson
Screening rates are abysmal. Only 8.3% of eligible smokers get screened. This is unacceptable. Rural areas lack facilities. Providers don't recommend it. Patients don't know. Systemic failures everywhere. Must improve access. Education is key. This is a national health crisis.
Jennifer Aronson
It's important to recognize that cultural factors play a role in screening disparities. In some communities, there's a mistrust of medical institutions due to historical injustices. This requires culturally competent outreach programs. Additionally, transportation barriers are significant in rural areas. Mobile screening units could help. Education about the benefits of early detection is crucial. We need to approach this holistically.
Kate Gile
Yes, the current situation is frustrating but we can do better. Let's focus on solutions: expanding Medicaid coverage for screening, training more providers to recommend it, and creating community health programs. Every step forward counts. We need to support each other in making this happen. It's possible!
Johanna Pan
Definitely agree with the solutions. We need to get the word out in communities. Maybe partner with local churches or community centers to spread awareness. Also, the government should fund more mobile clinics. Misspelling 'definitely' but you get the point. This is doable if we work together. Keep pushing!
Jenna Elliott
Only America has the resources to solve this. Other countries can't handle it. We need to export our screening protocols. Stop complaining and get it done. This is a national priority. No excuses.
Nancy Maneely
Exporting protocols is ridiculous. We have enough problems at home. Trying to fix other countries when we can't even get our own screening rates up is pure ignorance. We need to focus on fixing our own mess first. Stop being so arrogant. This is a disaster waiting to happen.
Albert Lua
Screening access varies globally, but we should share knowledge. Other countries have different healthcare systems but can learn from our experience. Collaboration is key. Let's work together to improve lung cancer outcomes worldwide. It's not just about America; it's about humanity.
Laissa Peixoto
It's interesting how nationalism overshadows public health. The real issue is systemic inequities within our own system. Before exporting anything, we need to fix the 8.3% screening rate. It's not about pride; it's about saving lives. Maybe we should look at how other countries handle similar issues. There's always room for improvement. Let's focus on the data, not the ego.
Lana Younis
Global collaboration is key but we need to tailor approaches. Each country has unique barriers. The US model isn't perfect but it's a good starting point. We should share best practices without imposing. Also, education is crucial for patients to understand screening benefits. Misspelling 'tailor' but you get it. Let's build bridges not walls. This is a team effort.