Many people over 65 take five or more medications every day. Some of them might not even need them anymore. But they keep taking them because no one ever asked if they still mattered. That’s not just a health risk-it’s a money drain. A $120-a-month sleep aid you haven’t needed in two years. A vitamin D supplement your blood tests showed you’re not deficient in. A pill for acid reflux your doctor prescribed five years ago and never checked on since. These aren’t just habits. They’re costs that add up-fast.
Why You’re Paying for Medications You Don’t Need
It’s not your fault. Doctors don’t sit down with you every year and say, “Let’s go through every pill in your cabinet.” Most visits are 15 minutes long. You mention your knee hurts. They write a new prescription. You mention your stomach feels off. Another pill gets added. Over time, your medicine cabinet becomes a cluttered list of things you started for one reason, but now serve no real purpose.
According to the American Geriatrics Society, 67% of hospital admissions for people over 85 involve medication-related problems. That’s not accidents or bad luck-it’s often the result of taking drugs that no longer help, or that actually cause harm. One study found that 37% of medication-related hospitalizations in older adults are preventable. And the financial toll? A single avoidable hospital stay costs an average of $15,700. Meanwhile, your monthly prescriptions? They’ve gone up 60% since 2014.
What Deprescribing Really Means
Deprescribing isn’t about quitting meds cold turkey. It’s not about ignoring your doctor. It’s a planned, safe process of stopping drugs that no longer do more good than harm. The term was formalized around 2012 by researchers in Canada and the U.S., and now it’s backed by the American Academy of Family Physicians, the American Geriatrics Society, and even Medicare.
Think of it like cleaning out your closet. You keep things because they “might come in handy.” But after a while, you realize you haven’t worn half of it in years. Deprescribing is the same. You look at each medication and ask: Is this still helping? Is it causing more problems than it solves? Can I stop it safely?
For example, proton pump inhibitors (PPIs)-drugs like omeprazole-are often prescribed for heartburn. But many people take them for years, even when they no longer have symptoms. A 2021 study showed that stopping these drugs saved patients an average of $420 a year-and lowered their risk of pneumonia by 25%. That’s not a coincidence. Long-term use can weaken bone density, increase infection risk, and cause nutrient deficiencies. The benefit? Gone. The cost? Still there.
How to Start the Conversation with Your Doctor
You don’t need to wait for a crisis. You can start this conversation today. But you have to come prepared. Most doctors won’t bring it up first. They’re busy. They’re not trained to audit your meds every visit. So you need to lead.
Here’s what to do before your next appointment:
- Collect every medication you take-prescription, over-the-counter, vitamins, supplements, even herbal teas or remedies. Put them all in a brown bag.
- Write down why you take each one. If you don’t know, write “I’m not sure.”
- Write down how much each costs per month. Don’t guess. Check your pharmacy receipt or log into your insurance portal.
- Make a list of side effects you’ve noticed: dizziness, fatigue, confusion, stomach upset, falls, trouble sleeping.
At your appointment, say this: “I’d like to review all my medications. I want to make sure I’m only taking what I still need. I’m worried about costs and side effects.”
Ask these five questions for every drug:
- Why am I taking this?
- What’s it supposed to do for me?
- Could it be causing dizziness, confusion, or falls?
- Can I stop it-or lower the dose?
- Who should I check in with if I feel different after stopping?
Doctors who use structured deprescribing tools like the Beers Criteria or the Medication Appropriateness Index (MAI) can quickly spot high-risk medications. The MAI takes about 7 minutes per pill to assess-but if you come prepared, your visit becomes more efficient. In fact, 68% of physicians say patients who bring a full list make deprescribing discussions much easier.
What Happens When You Stop a Medication?
You won’t just stop cold. That’s dangerous. For some drugs-like blood pressure meds, antidepressants, or steroids-stopping suddenly can cause rebound effects. Your blood pressure might spike. Your anxiety might return worse than before. Your stomach might start burning again.
That’s why deprescribing is slow. It’s usually one medication at a time. And it’s monitored. Your doctor might suggest cutting the dose in half for two weeks, then stopping entirely. Or switching to a lower-cost version. Or replacing it with a non-drug solution-like exercise for mild depression, or dietary changes for acid reflux.
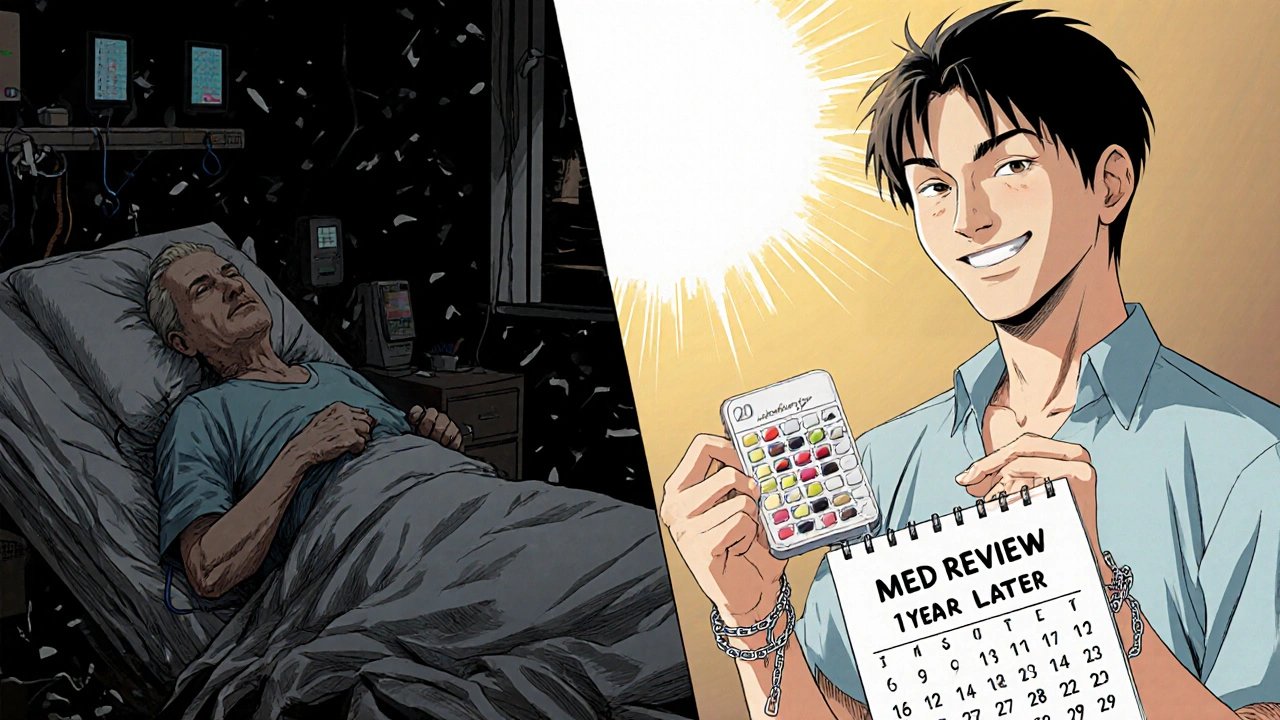
One woman from Ohio, 72, stopped three unnecessary meds after a brown bag review. She saved $840 a year. One was a $120/month sleep aid she hadn’t needed since her hip surgery. Another was a $40/month supplement her cardiologist said duplicated her prescription. The third was a daily aspirin she’d been taking since 2010-no one had ever asked if she still needed it.
On Reddit, a user named SeniorSaver87 cut out a $90/month vitamin D supplement (after a blood test showed normal levels) and a $75/month herbal remedy. That’s $1,980 saved in one year. No side effects. No complications. Just smart cleanup.
Where to Get Help Beyond Your Doctor
You’re not alone in this. Your pharmacist is a hidden ally. Under Medicare Part D, 85% of community pharmacies offer free Medication Therapy Management (MTM) services. That’s a 30- to 60-minute session where a pharmacist reviews all your meds, checks for interactions, and finds cheaper alternatives.
One 2022 study found pharmacists identified an average of $1,200 in annual savings per patient just by suggesting generic switches or stopping redundant drugs. And they’re trained to spot what doctors might miss-like taking three different painkillers that all contain acetaminophen, risking liver damage.
Also, check if your health plan offers a medication review program. Kaiser Permanente’s system reduced medication costs by $47 per member per month and cut adverse drug events by 28%. CMS now requires Medicare Part D plans to offer these services to high-risk patients. You don’t have to ask for it-call your plan and ask, “Do you offer a free medication review?”
What to Watch Out For
Deprescribing works-but only when done right. A 2022 survey by the National Council on Aging found that 18% of people who tried to stop meds on their own ended up in the ER or doctor’s office with side effects. That cost them an average of $1,200 in extra care. That’s worse than the original cost of the pill.
Never stop a medication without talking to your doctor. Especially not:
- Blood pressure or heart meds
- Antidepressants or anti-anxiety drugs
- Diabetes medications
- Steroids or seizure drugs
Even if you think it’s “just a vitamin,” don’t assume. Some supplements interact with prescriptions. St. John’s Wort, for example, can make blood thinners, birth control, and antidepressants less effective.
And don’t be afraid to say no. If your doctor says, “We’ll just keep it for now,” ask: “What’s the plan to check if I still need it?” If they can’t give you a clear answer, ask for a follow-up in three months. Write it down. Hold them to it.
How Much Can You Really Save?
Let’s do the math. If you’re taking three unnecessary medications that cost $50 a month each, that’s $1,800 a year. Eliminate one medication-related hospitalization, and you save $15,700. That’s not theoretical. It’s happening every day.
Kaiser Permanente’s program saved $1.2 million annually by reducing inappropriate meds in just one health system. The Lown Institute estimates inappropriate polypharmacy costs the U.S. $30 billion a year in avoidable hospital visits and ER trips. Medicare beneficiaries alone could save $2.8 billion a year if unnecessary prescriptions were stopped.
And it’s getting more urgent. Since 2014, drug prices have risen 3.4 times faster than inflation. Seniors on fixed incomes now spend 18.3% of their income just on prescriptions. That’s not sustainable. Deprescribing isn’t a luxury-it’s a financial necessity.
What’s Next?
This isn’t a one-time event. Medication needs change as you age, as your health changes, as new conditions appear or old ones fade. Schedule a medication review once a year. Do it after a hospital stay. Do it after a major life change-like retirement, moving, or losing a spouse.
And if your doctor says, “I don’t have time,” ask for a referral to a pharmacist who does. Or ask for a follow-up appointment specifically for meds. Most doctors will agree if you show you’ve done your homework.
You’re not asking to stop your care. You’re asking for smarter care. Less clutter. Less risk. Less cost. And better health.
What does it mean to deprescribe?
Deprescribing means safely stopping medications that are no longer needed or that do more harm than good. It’s not quitting drugs cold turkey-it’s a planned, gradual process done with your doctor’s guidance to reduce side effects, improve health, and lower costs.
Can I stop my meds on my own?
No. Stopping certain medications without medical supervision can cause serious harm-like rebound high blood pressure, seizures, or worsening anxiety. Always talk to your doctor or pharmacist first. Even if a pill seems harmless, like a vitamin or supplement, it could interact with other drugs you take.
How do I know if I’m taking too many meds?
If you take five or more medications daily, you’re at risk for polypharmacy. Signs you might be taking unnecessary drugs include: taking something because “you always have,” not knowing why you’re on it, experiencing side effects like dizziness or confusion, or paying over $100 a month for pills you don’t feel are helping.
Will my insurance cover a medication review?
Yes-if you’re on Medicare Part D, you’re eligible for free Medication Therapy Management (MTM) from your pharmacy. Many community pharmacies offer this service at no cost. Call your pharmacy and ask if they provide MTM. You don’t need a referral.
How long does it take to see savings after deprescribing?
You’ll see savings on your next prescription refill-often within 30 days. If you stop a $50/month drug, you save $600 a year. Avoiding one hospital visit due to a bad reaction can save $15,000 or more. The financial benefit starts immediately; the health benefits often show up within weeks.





Jefriady Dahri
This is gold. My dad took 12 pills a day until we did the brown bag thing. Turned out he didn’t need half of them. Saved $900/year and stopped falling so much. 🙌
Sharley Agarwal
I hate how doctors just keep prescribing. No one ever asks if you still need it.
Karen Willie
I wish more people knew about MTM services. My pharmacist caught three dangerous interactions I didn’t even realize were happening. Free, easy, life-changing.
Don’t wait until you’re in the ER to ask for help.
Arup Kuri
Big Pharma doesn’t want you to stop taking pills. They’re making billions off your confusion. Your doctor? They’re paid per script. It’s not about your health - it’s about profit. You’re being played. And don’t get me started on supplements - they’re all scams.
Elise Lakey
I’m scared to ask my doctor about deprescribing. What if they think I’m being difficult? Or worse - that I’m trying to skip necessary meds?
Patricia McElhinney
I'm sorry, but this article is dangerously oversimplified. You can't just 'stop a pill' because it's expensive. You're talking about people with complex comorbidities. One wrong decision and you're in the hospital. This is not a budgeting tip. It's medical malpractice waiting to happen.
Dolapo Eniola
In Nigeria we don’t even have access to half these meds. You people complain about $120/month sleep aids? We’re lucky to get a basic painkiller. This is a first-world problem dressed up as a revolution. 🤡
Agastya Shukla
The Beers Criteria and MAI are solid frameworks, but they’re not foolproof. Polypharmacy risk is non-linear - it’s not just about quantity. Pharmacokinetic changes in aging, renal clearance decline, and CYP450 polymorphisms all modulate drug response. You need individualized assessment, not a checklist.
Rachel Villegas
I did this last year. Stopped the aspirin, the melatonin, and the calcium supplement. No side effects. My pharmacy bill dropped by $600. I feel lighter. Like I finally stopped carrying around dead weight.
Shivam Goel
Wait - you’re telling me that a 72-year-old woman stopped three meds and saved $840? That’s statistically insignificant. The sample size is N=1. And you’re using anecdotal Reddit posts as evidence? Where’s the peer-reviewed data? The confidence intervals? The p-values? This is not science - it’s feel-good clickbait.
Archana Jha
They’re putting chemicals in your pills to keep you dependent. The FDA is in bed with the drug companies. They don’t want you to heal naturally. That’s why they never tell you about magnesium for sleep or turmeric for inflammation. You think this is about money? It’s about control.
Aki Jones
I’ve been reading about this for months. The truth is, they’re testing new drugs on elderly patients through ‘off-label’ prescriptions. That’s why they never stop anything. They’re using you as a guinea pig. And your doctor? They’re getting kickbacks. I’ve seen the documents.
Andrew McAfee
In my village in Ghana, we use neem leaves for blood pressure and ginger for digestion. We don’t need pills. But here? You’re told to swallow something for everything. We’ve lost touch with our bodies. This isn’t medicine - it’s consumerism.
Andrew Camacho
I had a heart attack last year. They gave me eight meds. I thought I was saved. Then I read this and asked my doc to cut them down. Two months later? I feel better than I have in ten years. I cried. Not from sadness - from relief. This isn’t just about money. It’s about getting your life back.