Getting the right dose of liquid medicine isn’t just about following the label-it’s about understanding exactly what it says. A wrong dose can make a child overly sleepy, cause nausea, or even lead to hospitalization. In the U.S., about 1.3 million injuries each year come from medication errors, and nearly half of those involve liquid prescriptions. The good news? Most of these mistakes are preventable if you know how to read the label correctly.
Why Milliliters (mL) Are the Only Unit You Should Trust
Look at the dose on your prescription label. If it says "5 mL," that’s what you use. If it says "1 teaspoon," stop. That’s outdated-and dangerous.
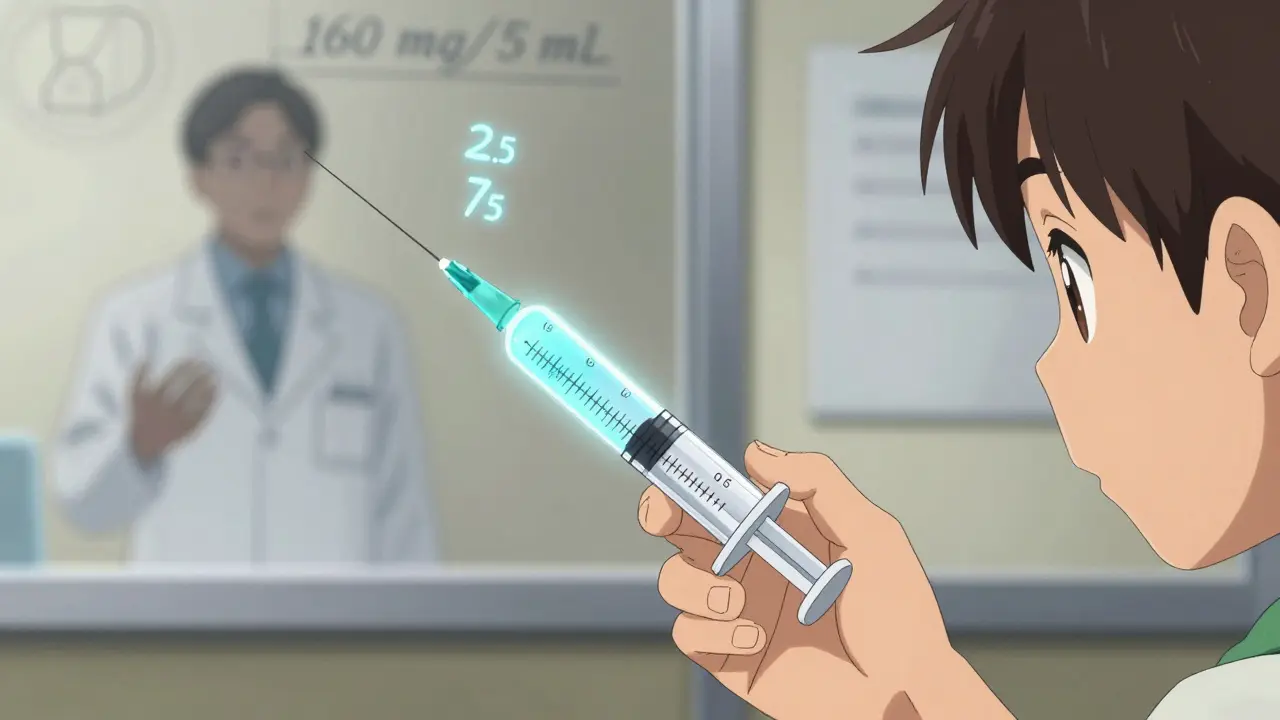
The FDA and the National Council for Prescription Drug Programs (NCPDP) have required pharmacies to use only milliliters (mL) since 2016. Why? Because teaspoons and tablespoons vary wildly. A kitchen teaspoon might hold anywhere from 2.5 to 7.5 milliliters. A tablespoon? It could be 5 mL or 20 mL. That’s a 300% difference. One study found parents using household spoons were twice as likely to give the wrong dose compared to those using mL-measured tools.
Even if your label has both mL and tsp, ignore the tsp. The only number you need is the one followed by "mL." The rest is there for backward compatibility, not safety. Always trust mL.
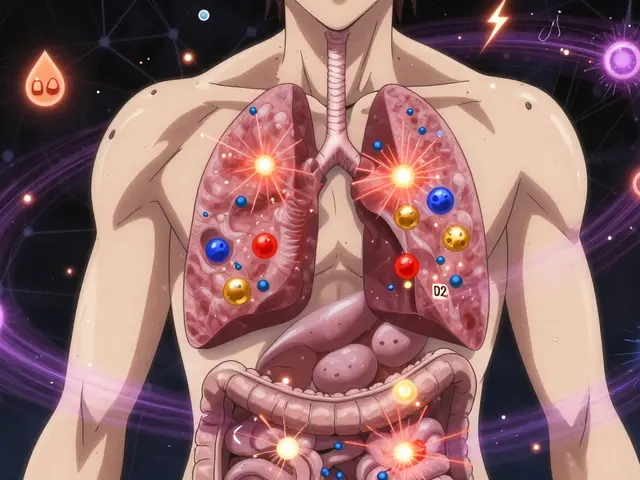
What the Concentration Really Means
Look for a line like this: 160 mg/5 mL. This isn’t just decoration. It tells you how much medicine is in each 5 milliliters. If your child needs 80 mg, you don’t give 5 mL-you give half of that, or 2.5 mL.
People often confuse the concentration with the total dose. For example, if the bottle says "160 mg/5 mL" and the label says "Take 5 mL," that means you’re giving 160 mg. But if the instruction says "Take 2.5 mL," you’re giving half that amount: 80 mg.
Here’s a quick way to check: divide the total dose needed by the concentration. Need 120 mg? The medicine is 160 mg per 5 mL. So: 120 ÷ 160 = 0.75. Multiply that by 5 mL → 3.75 mL. That’s your dose. If you’re unsure, ask your pharmacist to show you how to calculate it.
Decimal Points Can Kill
Pay attention to how numbers are written. If you see "0.5 mL," that’s half a milliliter. If you see ".5 mL," that’s the same thing-but it’s written wrong and dangerous.
According to Johns Hopkins research, writing doses like ".5 mL" (without the leading zero) leads to 10-fold dosing errors. Someone might misread it as "5 mL" and give ten times too much. That’s why FDA and NCPDP require 0.5 mL, never .5 mL.
And never write or read a dose like "5.0 mL." That trailing zero suggests precision that doesn’t exist in most liquid medications. It can trick you into thinking you need to measure exactly 5.0 instead of 5. The rule is simple: use leading zeros, never trailing zeros.
The Dosing Device Matters More Than You Think
Most prescriptions come with a dosing cup, syringe, or dropper. Don’t use a kitchen spoon. Don’t use a regular medicine cup if it’s not marked in mL. Even if the cup says "teaspoon," the mL markings are what count.
Check the device. Does it have clear lines for 0.5 mL, 1 mL, 2.5 mL, 5 mL? If it only has "tsp" or "tbsp," ask for a new one. Pharmacies are required to provide a measuring device that matches the label’s units. If they don’t, request one. Many pharmacies now offer free oral syringes-especially for children.
Some devices measure down to 0.01 mL. Others only go to 1 mL. If your dose is 1.2 mL and your syringe only has 1 mL and 2 mL marks, you’re stuck guessing. That’s why you should always use the device that came with the medicine. If you lost it, go back to the pharmacy and get a new one. They’ll give it to you for free.
Don’t Trust Your Memory-Use the Teach-Back Method
After the pharmacist gives you instructions, don’t just nod and walk away. Ask them to show you how to measure the dose. Then, do it yourself in front of them.
This is called the "teach-back" method. Studies show it reduces dosing errors by 63%. Say something like: "Can I show you how I’d give this to my child?" Then pick up the syringe, draw the correct amount, and point to the line. If they say, "Wait, that’s not right," you’ve just prevented a mistake.
Even if you think you understand, teach-back works. A 2021 study from Nationwide Children’s Hospital found that 78% of parents who demonstrated proper dosing made no errors later. Without it, the error rate was nearly 40%.

Watch Out for These Common Mistakes
- Mistaking total volume for dose: The bottle might say "120 mL"-that’s the total amount in the bottle, not how much to give. The dose is always on the instruction line.
- Reading "5 mL" as "50 mL": If the label is blurry or small, it’s easy to misread. Always hold the label up to good light. If you can’t read it clearly, call the pharmacy.
- Using expired medicine: Liquid medications often expire 14-30 days after opening, even if the bottle says "expire 2027." Check the label for "discard after" dates.
- Assuming all brands are the same: Children’s Tylenol and generic acetaminophen may have different concentrations. One might be 160 mg/5 mL; another might be 120 mg/5 mL. Never swap them without checking the concentration.
What’s New in 2026?
By 2026, most pharmacies will be required to include visual guides on liquid medication labels-small pictures showing how to draw up the dose. The FDA proposed this rule in 2023 after a study showed pictograms reduced errors by 37%.
Some pharmacies, like Amazon Pharmacy and McKesson’s Medly, are already adding QR codes that link to short videos showing exactly how to use the dosing device. If your label has a QR code, scan it. It might be the safest way to confirm you’re doing it right.
The American Academy of Pediatrics is also pushing for pediatricians to teach parents how to read labels during well-child visits. By 2026, you may no longer have to guess-your doctor might show you before you even leave the office.
What to Do If You’re Still Unsure
If you’re confused, call your pharmacy. Pharmacists are trained to explain this. Don’t feel embarrassed. Nearly 43% of patients misread even properly labeled prescriptions because of low health literacy.
Write down the dose, concentration, and frequency on a sticky note. Put it on the fridge. Show it to caregivers. If you’re giving medicine to a grandchild, make sure the babysitter knows how to read the label too.
And if you ever feel like you gave the wrong dose-call your doctor or poison control immediately. Don’t wait. It’s better to be safe than sorry.
Reading a liquid prescription label isn’t hard. But it requires attention. One extra second checking the mL, one extra minute asking for a syringe, one extra question to your pharmacist-those seconds save lives.




Mike Rose
why do they make this so hard? just give me a spoon and shut up.
Claire Wiltshire
It’s so important to emphasize that milliliters are the only safe unit-household spoons vary so much that even experienced caregivers can misjudge. I’ve seen parents use soup spoons because they didn’t know the difference, and it’s terrifying. Always use the syringe or cup provided, and if it’s missing, call the pharmacy. They’re legally required to give you one. Also, never ignore the leading zero: 0.5 mL, not .5 mL. That tiny detail saves lives.
April Allen
The concentration-to-dose conversion is where most cognitive load happens. The 160 mg/5 mL schema isn’t just a label-it’s a proportional relationship that requires basic algebraic reasoning. When parents don’t parse this, they default to volume-based heuristics, which is why the teach-back method is non-negotiable. It externalizes the cognitive burden and creates a feedback loop with the clinician. We need this embedded in all pediatric discharge protocols.
Sheila Garfield
I’ve been a nurse for 22 years and I still double-check every liquid med label. Even the ones I’ve given a hundred times. That’s not paranoia-that’s professionalism. And if you’re ever unsure? Call your pharmacist. They’re not just filling scripts-they’re your last line of defense. Seriously, don’t be shy. They’ve seen it all.
Sidhanth SY
Actually, in India we mostly get syringes with mL markings now, but I still see people using teaspoons because it’s ‘what they’ve always done.’ Maybe the real issue isn’t the label-it’s the habit. Education needs to start at home, not just at the pharmacy. A simple poster in the waiting room could help a lot.
Adarsh Uttral
lol i once gave my niece 5ml thinking it was 5 tsp and she was out cold for 3 hours. never again. always check the ml. also never trust the cup that came with it if it says tsp. just use a syringe.
Shawn Peck
THIS IS WHY AMERICA IS FALLING APART. PEOPLE CAN’T READ A LABEL. THEY USE KITCHEN SPOONS LIKE THEY’RE COOKING SOUP. THE FDA HAS TO HAND-HOLD EVERY SINGLE PERSON. I’M SO SICK OF THIS. IF YOU CAN’T MEASURE 2.5 ML, YOU SHOULDN’T BE PARENTING. STOP BEING LAZY.
Russ Kelemen
What struck me most isn’t the math or the units-it’s the fear. So many parents don’t ask because they’re afraid they’ll sound stupid. But this isn’t about intelligence. It’s about systems that assume everyone has the same access to information. The teach-back method isn’t just clinical-it’s human. It says: ‘I see you’re stressed. Let me help you feel safe.’ That’s the real medicine here.