When you pick up a generic prescription, you’re not getting a cheaper version of a drug-you’re getting the same drug, proven to work the same way. The FDA doesn’t allow generic manufacturers to cut corners. Every generic pill, injection, or inhaler must match the brand-name version in safety, strength, purity, and how your body absorbs it. This isn’t marketing. It’s science-and it’s tightly controlled.
What Makes a Generic Drug Approved?
The path to approval for a generic drug is called the Abbreviated New Drug Application, or ANDA. It’s called "abbreviated" because it doesn’t require repeating the full clinical trials done for the original brand-name drug. But don’t mistake "abbreviated" for "easy." The FDA still demands proof that the generic performs identically in your body. That means the same active ingredient, the same dose, the same way it’s taken-whether it’s a tablet, capsule, or injection.
Here’s what the FDA requires: the generic must have the same active pharmaceutical ingredient (API) as the brand-name drug. No substitutes. No variations. It must also match the dosage form-like a 10 mg tablet-and the route of administration-like oral or intravenous. Even the color, shape, or flavor doesn’t matter as long as it doesn’t affect how the drug works. The only thing that counts is whether your body gets the same amount of medicine, at the same speed, and for the same length of time.
Bioequivalence: The Core of Generic Approval
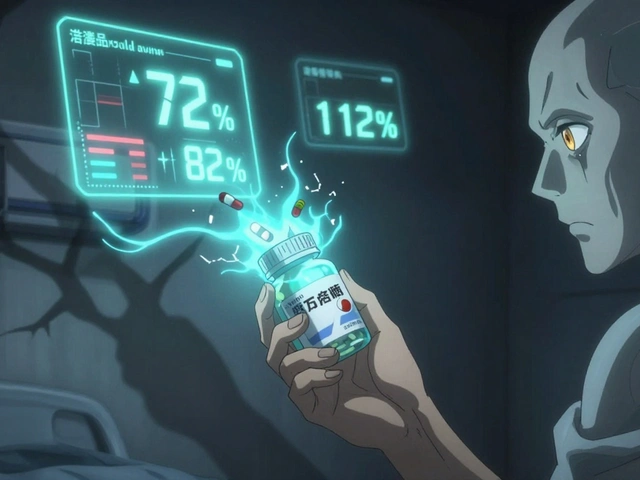
The most critical test for any generic drug is bioequivalence. This isn’t a guess. It’s a precise measurement. Researchers give the brand-name drug and the generic to healthy volunteers, then take blood samples over time to track how much of the drug enters the bloodstream and how fast.
The FDA requires the generic’s absorption to fall within 80% to 125% of the brand-name drug’s absorption. This range is based on decades of data showing that variations within this window don’t affect clinical outcomes. For example, if the brand-name drug delivers 100 units of medicine into your blood, the generic must deliver between 80 and 125 units. That’s it.
But not all drugs are treated the same. For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or lithium-the stakes are higher. A small difference in blood levels can cause serious side effects. For these, the FDA tightens the range. Levothyroxine generics, for instance, must stay within 95% to 105% of the brand’s absorption. That’s a much narrower margin, and manufacturers have to prove it with extra testing.
Strength, Purity, and Stability: Non-Negotiables
Strength isn’t just about how much medicine is in the pill. It’s about consistency. Every batch, every tablet, every capsule must contain the exact same amount of active ingredient. The FDA requires manufacturers to test each batch before release. If one tablet has 9.2 mg and another has 10.8 mg of the same drug, the batch gets rejected.
Purity matters too. The drug can’t have harmful impurities. Even trace amounts of contaminants from the manufacturing process must be below strict limits set by the FDA. These limits are based on toxicology studies and international standards. For example, nitrosamine impurities-linked to cancer in high doses-are now monitored in all new generic applications.
Stability is another key requirement. A generic drug must remain effective and safe throughout its shelf life. That means testing under different temperatures, humidity levels, and light exposure. Manufacturers must prove their product won’t break down or lose potency before the expiration date. If a generic tablet crumbles in a hot warehouse, it’s not approved.
Manufacturing: No Shortcuts Allowed
The FDA inspects every manufacturing facility-whether it’s in the U.S., India, or China-before approving a generic drug. These inspections are unannounced and thorough. The agency checks for compliance with Current Good Manufacturing Practices (cGMP), which cover everything from equipment cleaning to employee training.
One common failure point? Inconsistent tablet hardness. In 2021, the FDA rejected a generic version of Jardiance because tablet hardness varied across production batches. That might sound minor, but if a tablet is too hard, it won’t dissolve properly. Too soft, and it breaks apart in the bottle. Either way, your body won’t get the right dose.
Manufacturers must also validate their processes. The FDA expects data from at least three consecutive commercial-scale batches showing the same quality, strength, and purity. This isn’t a lab experiment-it’s real production. And if the facility fails an inspection, approval is delayed until the issues are fixed and re-inspected.
Complex Generics: Where Approval Gets Harder
Not all generics are created equal. Simple pills? Easy. Inhalers, eye drops, topical creams, or long-acting injectables? Much harder. These are called complex generics, and they’re the biggest challenge in the approval process.
Take the EpiPen. It’s not just about the epinephrine-it’s about the auto-injector device. The needle depth, spring force, and delivery timing all matter. Between 2015 and 2020, the FDA approved only 3 out of 27 generic EpiPen applications because the device didn’t match the original. The same goes for inhalers like Advair or asthma nebulizers. The drug is only half the battle. The delivery system has to work the same way.
That’s why complex generics take longer. On average, they take 47 months to get approved, compared to 28 months for simple pills. And rejection rates are higher. Only 58% of complex generic applications get approved within three review cycles, compared to 76% for conventional ones.
Why Do Some Generics Get Rejected?
Most rejections aren’t because the drug doesn’t work. They’re because the paperwork is incomplete, the manufacturing process isn’t well documented, or the bioequivalence data is shaky. The FDA’s review team uses a system called Question-Based Review (QbR) to dig into every detail. They ask: How was the drug formulated? How was the stability tested? What controls are in place to prevent contamination?
One 2023 survey of generic manufacturers found that 68% of applicants struggled most with designing bioequivalence studies. Another 45% had issues during FDA inspections. Many new companies underestimate how detailed the documentation needs to be. A typical ANDA submission can be 5,000 to 10,000 pages long. It’s not just a form-it’s a scientific dossier.

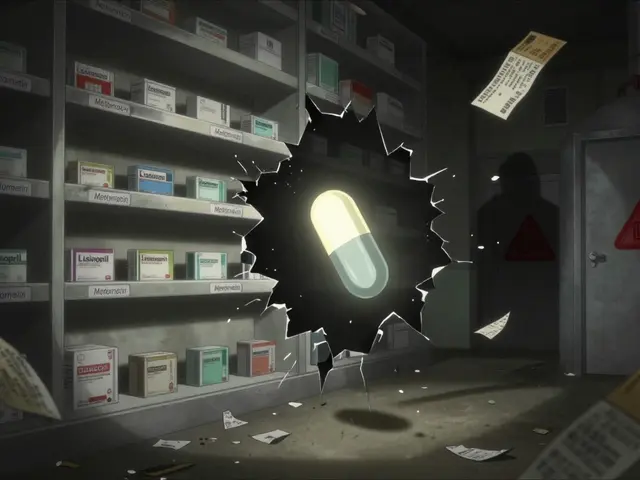
Cost, Speed, and Market Impact
Developing a brand-name drug can cost over $2.6 billion. A generic? Around $1.3 million. That’s why generics make up 90% of prescriptions in the U.S. but only 23% of total drug spending. In 2022 alone, generics saved the U.S. healthcare system $373 billion.
The FDA approved 90 generic drugs in 2023, including the first generic of Humira, a blockbuster biologic drug that had no competition for over a decade. But even with approval, market entry can be delayed. Patent lawsuits, settlement deals, and "evergreening" tactics by brand-name companies often push back generic launches by years. The FTC found an average delay of 2.4 years between FDA approval and when the generic actually hits pharmacy shelves.
Are Generics Really the Same?
Yes. The American Medical Association reviewed 15 years of real-world data and found that generics performed just like brand-name drugs in 98.7% of cases. Studies show no difference in hospitalizations, side effects, or treatment failure rates.
Some patients report feeling different on a generic. That’s usually because they’re switching from one brand to another, or from brand to generic, and their body is adjusting. It’s not the drug-it’s the change. Doctors often recommend staying on the same version once you’ve found what works.
The FDA’s own director of generic drugs, Sally Choe, says it plainly: "Every approved generic meets the same rigorous standards as the brand-name drug. There are no clinically meaningful differences."
What’s Changing in 2025?
The FDA is pushing to speed up approvals for complex generics. By 2027, they aim to approve half of these harder-to-make drugs within two review cycles-up from just 28% today. They’re also expanding their product-specific guidance documents to over 3,000 brand-name drugs, giving manufacturers clearer rules to follow.
And with more complex drugs losing patent protection-like injectables for diabetes, autoimmune diseases, and mental health-there’s a growing wave of generic applications coming. The FDA has identified 127 such drugs with no generic alternatives, representing $52 billion in annual sales. That’s not just opportunity. It’s a need.
Generics aren’t second-choice medicine. They’re the backbone of affordable healthcare. And the system that approves them is built on science, not savings. Every pill you take-no matter the price tag-has passed the same test.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires every generic drug to meet the same safety, strength, quality, and purity standards as the brand-name version. Generics use the same active ingredient and are tested in the same way. Post-market surveillance over 15 years shows no meaningful difference in safety or effectiveness between generics and brand-name drugs.
Why do some generics cost more than others?
Price differences between generics usually come from manufacturing costs, supply chain issues, or market competition-not quality. If a generic is made by a smaller company with higher production costs, or if there’s low competition for that drug, the price may be higher. But the FDA ensures all approved generics meet the same standards, regardless of price.
Can a generic drug have different inactive ingredients?
Yes. Generics can use different fillers, dyes, or preservatives than the brand-name drug. These are called inactive ingredients and don’t affect how the medicine works. But if they could impact absorption or cause an allergic reaction, the FDA requires the manufacturer to prove they’re safe and won’t interfere with the drug’s performance.
How long does it take to get a generic drug approved?
For simple pills, it takes about 28 to 33 months from submission to approval. Complex generics-like inhalers or injectables-can take 47 months or longer. The FDA has a goal to reduce this time, especially for complex products, and offers pre-submission meetings to help manufacturers avoid delays.
What happens if a generic drug fails FDA inspection?
If a manufacturing facility fails an FDA inspection, the application gets a Complete Response Letter. The company must fix the issues-like cleaning procedures, equipment calibration, or documentation gaps-and request a re-inspection. Approval is delayed until the FDA confirms the problems are resolved. In some cases, companies abandon the application if the cost of fixes is too high.
Generic drugs are one of the most successful public health innovations in modern medicine. They save billions every year and make essential treatments accessible to millions. Behind every low-cost pill is a rigorous, science-based approval process that doesn’t compromise on safety or quality.



Christina Bischof
Been on generics for years and never had an issue. My blood pressure med works the same as the brand and costs a third. Simple as that.
Nupur Vimal
Fact is most generics are made in India and China where quality control is a joke. I don't trust anything that's not made in America. The FDA is just rubber stamping now to save money. You think they really inspect every factory? Please.
Mike Nordby
The bioequivalence range of 80–125% is statistically robust and grounded in pharmacokinetic modeling. For narrow-therapeutic-index drugs, the FDA applies tighter thresholds, often 90–111% or even 95–105% as with levothyroxine. This isn't arbitrary-it's evidence-based. The real issue is inconsistent labeling and patient perception, not drug performance.
Cassie Henriques
Just read the ANDA submission for that new generic EpiPen-5000+ pages of device validation data. The spring force calibration alone had 17 different test protocols. It’s insane how much work goes into making something that looks like a plastic pen. And yeah, most get rejected. The tech is way harder than people think.
Jake Sinatra
Generics are essential. They’re not just cost-saving-they’re life-saving. Without them, millions wouldn’t be able to afford insulin, antiretrovirals, or antihypertensives. The science is solid. The system works. The only thing broken is the pricing structure that still lets brand-name companies profit from patents long after they should’ve expired.
RONALD Randolph
I don't care what the FDA says-I’ve seen people get sick on generics. My cousin had a seizure after switching. The FDA is corrupt. They’re owned by Big Pharma and Big Pharma owns the generic companies too. It’s all a scam. You think they’d let Chinese factories make our medicine? NO WAY. We need American-made drugs. Period.
Melissa Taylor
My mom’s on levothyroxine and they switched her to a generic last year. She’s been stable for 14 months now. Same labs, same energy, same no side effects. The science is there. Trust the data, not the fear.
Jocelyn Lachapelle
People worry about generics because they don’t understand how the system works. It’s not magic. It’s chemistry. It’s physics. It’s hundreds of tests done in labs across the world, all reviewed by scientists who don’t care if it’s made in Ohio or Odisha. What matters is whether your body gets the same dose, at the same rate, for the same time. And guess what? It does. Every single time. The real hero here isn’t the brand name-it’s the regulator who won’t cut corners. We should be shouting about this, not doubting it.