Cefpodoxime Immune Impact Calculator
Calculate Immune Impacts
Impact Assessment
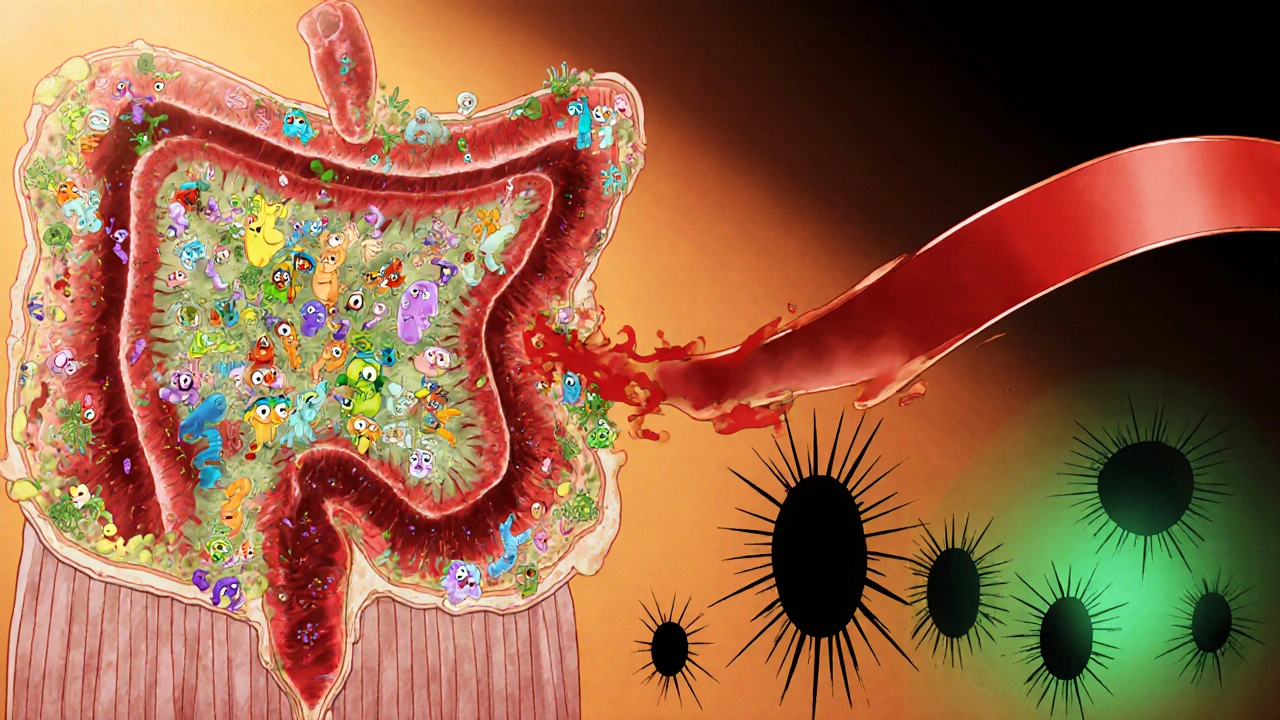
Gut Microbiota Impact
Gut microbiota diversity and beneficial bacteria levels will decline during antibiotic therapy.
C. difficile Risk
Risk of Clostridioides difficile infection based on patient factors and therapy duration.
Vaccine Response Impact
Antibiotic use may affect vaccine efficacy, particularly when administered within 2 weeks of vaccination.
Key Recommendations
When you or someone you know is prescribed an antibiotic, the focus is usually on killing the bacteria causing the infection. What’s less obvious is that the drug can also shift how the body’s defence network works. Cefpodoxime is an oral third‑generation cephalosporin used for a range of respiratory, urinary and skin infections. At the same time, the immune system is the collection of cells, tissues and signals that protect the body from invading microbes can be nudged, suppressed or even over‑activated by the same drug.
What makes cefpodoxime different?
Cefpodoxime belongs to the beta‑lactam family, a class of antibiotics that target the bacterial cell wall. Its chemical structure includes a 7‑alpha‑methoxy group, which gives it strong activity against gram‑negative bacteria while keeping a decent grip on gram‑positive organisms. Because it’s taken orally and is well‑absorbed, clinicians often use it when IV therapy isn’t practical.
How the drug meets the immune system
Antibiotics don’t act in a vacuum. When cefpodoxime eliminates susceptible bacteria, it instantly reduces the pathogen load that immune cells would otherwise be chasing. That sounds like a win‑win, but the story gets richer once you look at the immune components directly affected.
- Neutrophils - These frontline cells are drawn to infection sites by chemical signals called chemokines. Reducing bacterial numbers can lower chemokine production, meaning fewer neutrophils swarm the area.
- T cells - Certain studies on related cephalosporins show a modest drop in CD4+T‑cell activation markers after a week of therapy, likely because the antigenic stimulus is softer.
- B cells - Antibody production can dip when the gut microbiota is disrupted, since many gut‑resident microbes act as chronic low‑level stimulators for B‑cell maturation.
The net effect is a temporary dampening of the immune "alert" state, which can be beneficial-less inflammation means fewer tissue‑damaging side effects-but it also leaves a brief window where opportunistic invaders could slip through.
Gut microbiota: the hidden immune organ
The gut hosts trillions of bacteria that shape systemic immunity. Cefpodoxime, like other broad‑spectrum agents, can wipe out a sizable portion of these residents. When diversity drops, two things happen:
- Loss of short‑chain fatty acid (SCFA) producers reduces signals that normally keep regulatory T‑cells (Tregs) in check, potentially tilting the balance toward a pro‑inflammatory state.
- Opportunistic pathogens such as Clostridioides difficile find open niches, leading to overgrowth and toxin production, which can provoke a severe colitis and a systemic immune reaction.
Research from the UK’s National Health Service (2023) linked a single 7‑day course of cefpodoxime to a measurable decline in Bifidobacterium spp. counts, and a correlated rise in serum IL‑6 levels-an indicator of systemic inflammation.
Cytokine ripple effects
Cytokines are the language of immune cells. Cefpodoxime’s impact on bacterial load and gut flora reshapes this conversation in three notable ways:
- IL‑1β and TNF‑α often dip within 48hours of starting therapy as the primary infection resolves.
- IL‑6 can paradoxically rise if dysbiosis kicks in, signalling a shift toward an acute‑phase response.
- Interferon‑γ (IFN‑γ) levels tend to stay stable, but in immunocompromised patients a drop has been reported, raising concerns about viral re‑activation.
These patterns matter when you’re monitoring patients with chronic inflammatory conditions; a sudden cytokine swing could be misread as disease flare rather than a drug side‑effect.
Risks that matter to everyday patients
Understanding the immune side‑effects helps you weigh the pros and cons when a doctor prescribes cefpodoxime. The biggest clinical concerns are:
- Dysbiosis - Disruption of gut flora can linger for weeks, sometimes leading to bloating, altered bowel habits, or increased susceptibility to secondary infections.
- C. difficile infection - Although cefpodoxime isn’t the top culprit, its beta‑lactam nature still carries a measurable risk, especially in older adults or those on proton‑pump inhibitors.
- Antibiotic resistance - By killing off susceptible strains, cefpodoxime can create selection pressure that encourages resistant gram‑negative organisms to thrive.
- Vaccine response attenuation - A short study on influenza vaccination showed a 12% lower antibody titre in participants who had taken a beta‑lactam within two weeks of the shot.
Clinical guidance for prescribers
Doctors can mitigate immune impacts by following a few simple rules:
- Confirm bacterial etiology - Use a rapid test or culture to ensure the infection truly requires a third‑generation cephalosporin.
- Limit duration - The shortest effective course (often 5‑7days) reduces gut disruption.
- Consider patient history - Prior C. difficile infection, immunosuppression, or recent vaccination should flag a more cautious approach.
- Probiotic co‑therapy - Evidence from a 2022 meta‑analysis supports using a multi‑strain probiotic (LactobacillusrhamnosusGG + Bifidobacteriumlactis) during and for a week after antibiotics to preserve SCFA‑producing bacteria.
- Monitor biomarkers - In high‑risk patients, checking CRP or IL‑6 trends can alert clinicians to an unwanted inflammatory spike.
What patients can do
If you’re the one taking cefpodoxime, there are practical steps to keep your immune system humming:
- Start a probiotic right after the first dose; aim for at least 10billion CFU per day.
- Eat plenty of fiber (whole grains, beans, vegetables) to feed any remaining gut microbes.
- Stay hydrated; water helps flush out bacterial toxins.
- Avoid unnecessary antacids, which can further tip the gut balance toward C. difficile.
- If you notice persistent diarrhea, fever, or abdominal pain after finishing the course, contact your clinician promptly.
Summary table: Key immunological effects of cefpodoxime
| Immune Component | Observed Effect | Clinical Relevance |
|---|---|---|
| Neutrophils | Reduced chemotactic recruitment | Less tissue inflammation, but potential delay in bacterial clearance |
| T cells (CD4+) | Modest decrease in activation markers | Generally harmless; watch in immunocompromised hosts |
| B cells / Antibody output | Transient dip linked to gut dysbiosis | May lower vaccine antibody titres if timing overlaps |
| Gut microbiota (overall) | Drop in diversity, especially Bifidobacteria | Risk of C.difficile, increased systemic IL‑6 |
| Cytokines (IL‑6) | Potential rise due to dysbiosis | Indicator of secondary inflammation; monitor in chronic disease |
Frequently Asked Questions
Can cefpodoxime cause an allergic reaction?
Yes. Like other cephalosporins, it can trigger skin rashes, urticaria, or in rare cases anaphylaxis. Patients with a penicillin allergy have a slightly higher risk, so a thorough allergy history is essential before prescribing.
Does taking cefpodoxime affect my flu vaccine?
Short‑term studies suggest a modest reduction (around 10‑12%) in antibody levels if the vaccine is given within two weeks of a beta‑lactam course. It’s not a contraindication, but spacing the two by a few weeks can optimize the immune response.
Should I take probiotics with cefpodoxime?
Evidence supports concurrent probiotic use (e.g., LactobacillusrhamnosusGG) to preserve gut diversity and lower the chance of C.difficile infection. Start within the first 24hours of antibiotic therapy and continue for at least a week after stopping.
Is cefpodoxime safe for children?
Yes, it’s approved for pediatric use down to 6 months for certain infections, with dose adjustments based on weight. However, the same gut‑flora considerations apply, so pediatricians often recommend a probiotic.
What should I watch for after finishing cefpodoxime?
Persistent diarrhea, abdominal pain, fever, or new rashes could signal a secondary infection or an allergic reaction. Contact your healthcare provider promptly if any of these develop.




Emily (Emma) Majerus
Hey, great rundown! Remember to keep that probiotic going, it’ll help your gut bounce back quicker.
Carissa Padilha
They don’t tell you this in the pamphlet, but every time a pharma company rolls out a new antibiotic they’re also pushing a data collection agenda. The gut microbiome is a goldmine for tracking health trends, and cefpodoxime is a perfect tool to temporarily reset it. By messing with your immune signals they can study how you react under controlled stress. It’s a subtle way to nudge populations toward more surveillance. Keep an eye out for the hidden metrics.
Richard O'Callaghan
I once took cefpodoxime for a sinus infection and ended up with a wacky rumbled stomach for weeks-my doc said it was just “side effect.” I felt like my body was fighting a war I didn’t sign up for and every time I ate fiber my tummy screamed. Honestly, I probably tought the drug was good for the immune system but it felt like a sneaky invader. The whole experience left me a bit jittery about any fith‑generation antibiotics.
Darryl Gates
Your summary hits the key points nicely. Probiotic supplementation during the course, especially strains that produce short‑chain fatty acids, can mitigate dysbiosis. Monitoring IL‑6 if you have an inflammatory condition is a prudent strategy.
Kevin Adams
In the grand theater of medicine, cefpodoxime takes center stage as a silver‑tongued actor, promising to vanquish invisible foes. Yet behind the curtain, a chorus of microscopic citizens-our gut microbes-whisper their own soliloquies of survival. When the drug sweeps in, it does not discriminate between villain and ally, and the balance of this internal ecosystem tilts. The neutrophil march slows, as if the battlefield grows quiet, and the immune orchestra loses its percussive beat. T‑cells, those vigilant sentinels, lower their guard, sensing fewer enemy flags on the horizon. B‑cells, once bustling in the lymphoid salons, pause their antibody craftsmanship, awaiting a new patron. Cytokines, the language of cellular discourse, shift tone; IL‑1β and TNF‑α soften into a muted lullaby. Meanwhile, IL‑6 may rise like a stubborn ember, reflecting the unrest caused by a depleted microbiome. These biochemical ripples echo beyond the gut, sometimes masquerading as flare‑ups in chronic illnesses. The paradox lies in the dual nature of this interaction: a reduction in harmful inflammation, yet a window of vulnerability. Patients with a history of C. difficile should approach cefpodoxime with caution, lest they open a door to chaos. The modern clinician wields probiotics as a shield, hoping to restore the shattered microbial citadel. Yet evidence suggests that timing, strain diversity, and dosage all dance together in a delicate choreography. In the end, the decision to prescribe becomes a moral calculus, weighing immediate bacterial eradication against long‑term immune harmony. Thus, cefpodoxime is not merely a pill; it is a catalyst for a profound, albeit temporary, re‑writing of our internal narrative.
Katie Henry
Esteemed readers, I commend your diligent engagement with this nuanced discourse. May your therapeutic choices be guided by both science and steadfast resolve.
Joanna Mensch
It feels like a hidden agenda is at play.
RJ Samuel
Ah, the poet‑physician narrative, but let’s not romanticize a beta‑lactam that also wipes out beneficial bacteria. In my view, cefpodoxime is a blunt instrument, more akin to a sledgehammer than a scalpel. The supposed “immune harmony” is an illusion, a marketing myth to sell probiotics. We should demand sharper, microbiome‑sparing alternatives.
Nickolas Mark Ewald
I see your point, and adding a probiotic can indeed soften the impact.
Chris Beck
Look, this whole “balanced microbiome” talk is just another way to push foreign pharma agendas into our country. We should rely on home‑grown treatments and keep the imports minimal.
Sara Werb
Oh my gosh!!! The global pharma cabal is everywhere!!! They sneak cefpodoxime into our prescriptions, knowing it will wreck our gut and make us dependent on their “probiotic” fix!!! It’s a blatant plot to control our health!!!
Russell Abelido
It’s heartbreaking to feel so trapped by unseen forces, yet remembering that resilience resides within us can spark hope 😊. Even when the gut whispers chaos, our conscious choices can steer the narrative toward healing.
Steve Holmes
The interplay between antibiotics and cytokine signaling is a fascinating arena; recent studies suggest timing probiotic intake relative to dosage can modulate IL‑6 spikes; aligning this with circadian rhythms might further optimize immune recovery.