Not all medicines are created equal-even when they do the same job. You might think a generic pill is just a cheaper version of the brand-name one, but the story behind side effects is far more complicated. Whether you’re taking a prescription antibiotic, an over-the-counter painkiller, or a herbal supplement bought online, each class of medication comes with its own set of risks. And those risks aren’t always obvious.
Prescription vs. Generic: The Same Drug, Different Risks
The FDA says generic drugs must be identical to brand-name drugs in active ingredient, strength, dosage, and how they work in the body. That’s true. But what they don’t tell you is that the inactive ingredients can be completely different. These are the fillers, dyes, and preservatives that hold the pill together. For most people, they’re harmless. For others, they’re a problem. Take lactose. It’s a common filler in many generic medications. If you’re lactose intolerant, taking a generic version of your blood pressure pill could mean bloating, cramps, or diarrhea-not because the drug isn’t working, but because of the filler. Same goes for aspartame, sulfites, or soya lecithin. If you’ve ever had an unexpected reaction after switching to a cheaper version of your medicine, it might not be the drug at all. It’s the packaging. And then there are the narrow therapeutic index (NTI) drugs. These are medications where even a tiny change in blood levels can cause serious harm. Levothyroxine for thyroid conditions and warfarin for blood thinning fall into this category. Studies show that switching between different generic versions of these drugs-even ones approved by the FDA-can lead to unstable hormone levels or dangerous bleeding. That’s why many doctors recommend sticking with the same manufacturer. If your pharmacy switches your levothyroxine brand without telling you, your TSH levels could swing out of range. You might feel fine, but your body isn’t.Herbal Supplements: Just Because It’s Natural Doesn’t Mean It’s Safe
The word "natural" is a red flag in medicine. People assume herbal remedies are harmless because they come from plants. But plants are powerful. Echinacea, for example, is marketed for colds, but it can trigger asthma attacks, hives, and muscle pain. Feverfew, often taken for migraines, has been shown in animal studies to cause uterine contractions-so it’s dangerous during pregnancy. And St. John’s Wort? It’s a popular mood booster, but it can cause serotonin syndrome when mixed with antidepressants. Symptoms include high fever, tremors, confusion, and even death. Here’s the kicker: supplements aren’t regulated like prescription drugs. The FDA doesn’t test them for safety or effectiveness before they hit the shelf. A 2023 report from Medical News Today found that nearly 1 in 5 herbal products contain unlisted pharmaceuticals-like hidden statins or steroids. You think you’re taking chamomile tea for sleep. You’re actually taking something that could interact with your blood thinner and send you to the ER. Even common herbs like ginkgo, garlic, and ginger can increase bleeding risk when taken with warfarin or aspirin. And if you’re on antibiotics? Echinacea and goldenseal can interfere with liver enzymes, making your meds less effective-or more toxic. Yet most patients don’t tell their doctors they’re taking supplements. They don’t think it counts as "medicine."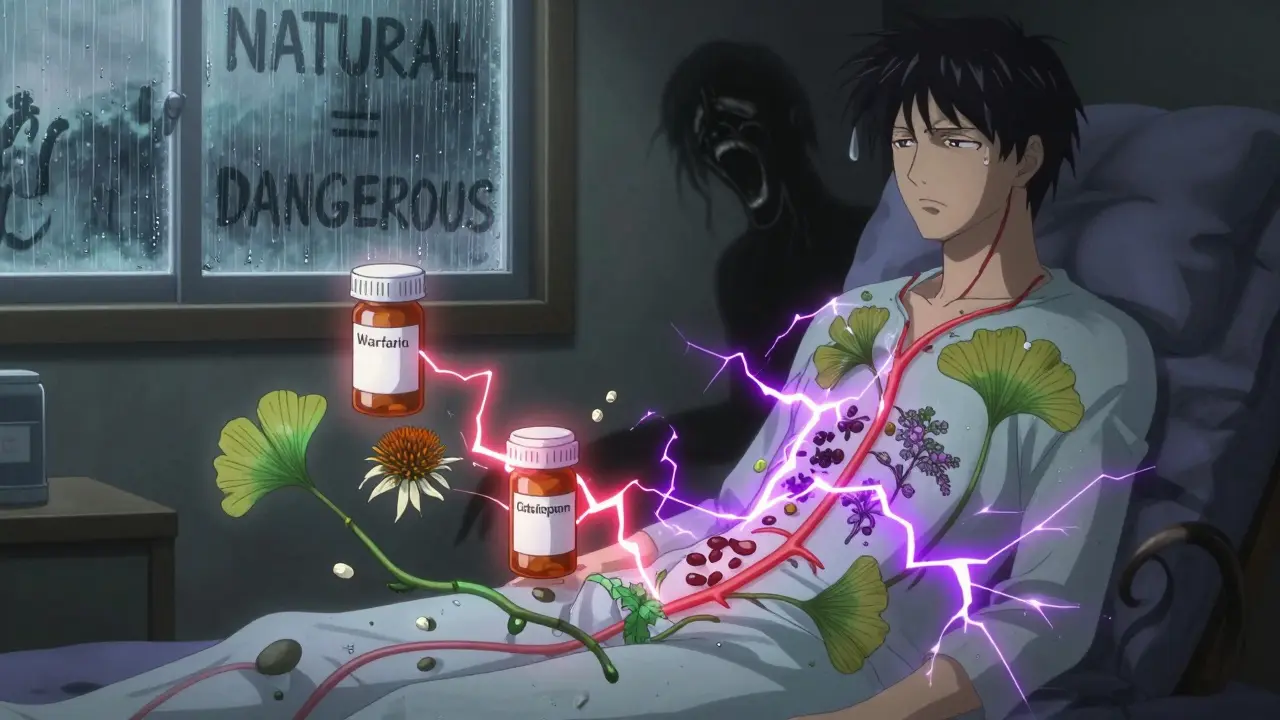
OTC Painkillers: The Silent Danger in Your Medicine Cabinet
Ibuprofen, acetaminophen, naproxen-these are the go-to pills for headaches, back pain, or fever. But they’re not harmless. Acetaminophen is the leading cause of acute liver failure in the U.S. when taken in excess, even slightly over the recommended dose. People don’t realize that many cold and flu meds already contain acetaminophen. Taking an extra Tylenol on top of that? That’s how overdoses happen. Ibuprofen and naproxen are NSAIDs. They can cause stomach ulcers, kidney damage, and raise blood pressure. Long-term users often don’t know they’re at risk until they start having black stools or swelling in their ankles. And here’s something few people consider: mixing OTC painkillers with alcohol. Even one drink with an NSAID can irritate the stomach lining. With acetaminophen? That combination can fry your liver. And don’t forget the silent interactions. Antihistamines in allergy meds can make you drowsy-dangerous if you’re driving or operating machinery. Decongestants like pseudoephedrine can spike blood pressure, which is risky if you have heart disease. These aren’t rare side effects. They’re common. And they’re preventable-if you read the label.Why Switching Medications Can Backfire
Insurance companies push generics because they’re cheaper. Pharmacies automatically substitute them unless you say "no." But for some patients, that switch isn’t harmless. A 2008 study found that patients with epilepsy who switched from brand-name to generic antiseizure drugs had more seizures and needed more doctor visits. The cost of those visits outweighed the savings on the pill. Even in cardiovascular drugs-where generics are most commonly used-some patients report worsening symptoms. One case cited by GoodRx involved someone switching from Celexa (brand) to citalopram (generic) for depression. Their anxiety spiked, sleep worsened, and they felt emotionally flat. Their doctor assumed it was their condition returning. It wasn’t. It was the inactive ingredients. The truth? Most people switch without issue. But for a small group, the difference matters. And if you’re one of them, you might not know why until it’s too late. That’s why it’s crucial to track how you feel after any switch. Keep a simple journal: date, medication, dose, and how you felt physically and mentally. Bring it to your next appointment.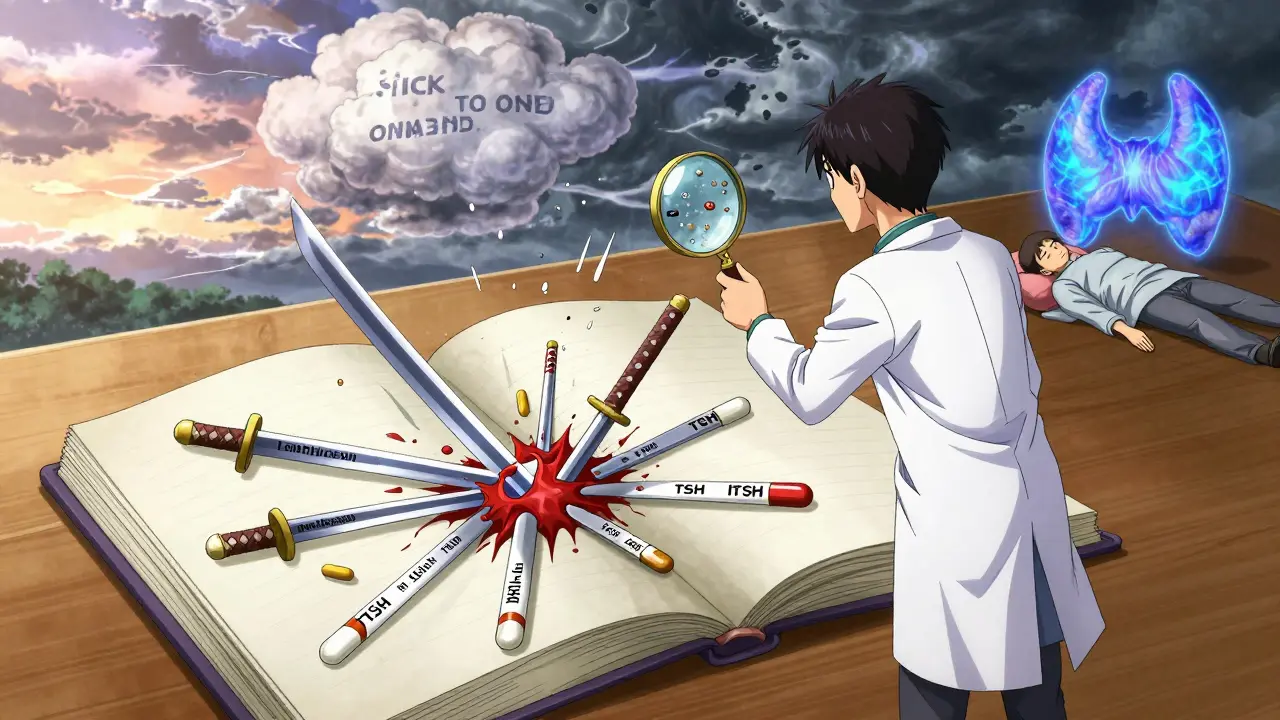
What You Should Do Right Now
Here’s what works in real life:- Check the inactive ingredients on every prescription label. If you’re allergic to lactose, soy, or dyes, ask your pharmacist for a version without them.
- Never mix supplements with prescriptions without checking. Tell your doctor or pharmacist everything you take-even gummy vitamins or herbal teas.
- Stick with one manufacturer for NTI drugs like levothyroxine or warfarin. Don’t let your pharmacy switch brands unless your doctor approves.
- Read OTC labels like a detective. Look for hidden ingredients. If you’re taking three different meds, check for overlap.
- Limit alcohol when on any medication. It doesn’t just make you sleepy-it can turn a safe drug into a dangerous one.
When to Call Your Doctor
You don’t need to panic over every little change. But if you notice any of these after starting or switching a medication, call your provider:- New rash, swelling, or trouble breathing
- Unexplained fatigue, dizziness, or confusion
- Black, tarry stools or unusual bleeding
- Worsening of your original condition
- Any new symptom you can’t explain
Are generic drugs always safe to switch to?
For most medications, yes. Generic drugs are required to have the same active ingredient and work the same way as brand-name versions. But for narrow therapeutic index (NTI) drugs like levothyroxine or warfarin, even small differences in absorption can cause problems. In these cases, staying on the same manufacturer’s version is safest. Always check with your doctor before switching.
Can herbal supplements really interact with prescription drugs?
Absolutely. St. John’s Wort can make antidepressants, birth control, and blood thinners less effective-or cause dangerous serotonin buildup. Echinacea can interfere with liver enzymes, changing how your body processes other meds. Ginkgo, garlic, and ginger can increase bleeding risk when taken with warfarin or aspirin. Many patients don’t tell their doctors about supplements because they think they’re harmless. They’re not.
Why do some people have side effects from generics but not brand-name drugs?
It’s usually not the active ingredient-it’s the fillers. Lactose, dyes, or preservatives in generics can trigger reactions in people with allergies or intolerances. One person might tolerate a generic just fine, while another breaks out in hives or gets stomach cramps. Always check the inactive ingredients list on the label. If you’ve had a reaction before, ask your pharmacist for a version without those additives.
Is it safe to take OTC painkillers every day?
Not long-term. Daily use of ibuprofen or naproxen can damage your stomach lining, kidneys, or raise blood pressure. Acetaminophen, even at normal doses, can cause liver damage if taken with alcohol or over several days. These aren’t candy. Use them only as needed, and never exceed the maximum daily dose. If you’re taking them daily for chronic pain, talk to your doctor about safer long-term options.
Should I stop taking supplements if I’m on prescription meds?
Not necessarily-but you should talk to your doctor first. Some supplements are fine. Others can be dangerous. The key is disclosure. Many drug interactions happen because patients don’t mention they’re taking turmeric, fish oil, or melatonin. Your doctor can’t protect you if they don’t know what you’re using. Make a list of everything you take and review it at every appointment.
How do I know if a side effect is from the drug or my condition?
It’s often hard to tell. A rash could be from an antibiotic-or from the infection you’re treating. Fatigue might be from your thyroid meds-or from your thyroid condition itself. The best approach is timing. Did the symptom start after you began the new medication? Did it improve when you stopped it? Keep a symptom diary and share it with your provider. They can help you connect the dots.





Rosemary O'Shea
Oh, sweet mercy, people still think 'natural' means safe? I once had a client who took 'organic' turmeric capsules with warfarin and ended up in the ER with internal bleeding. She swore it was 'just a supplement.' Honey, if it alters your biochemistry, it’s a drug. Stop romanticizing plants-they don’t care if you live or die.
And don’t get me started on pharmacies auto-switching levothyroxine brands. My TSH went from 2.1 to 8.9 in two weeks because some intern at CVS thought 'generic' meant 'interchangeable.' I had to call my endocrinologist in tears. The FDA doesn’t regulate the fillers. That’s not a loophole-it’s a death sentence waiting to happen.
And yes, I keep a spreadsheet. Date, med, dose, mood, bowel movements. Because if you’re not tracking it, you’re just guessing. And guessing with your thyroid? That’s not bravery. That’s negligence.
Also, St. John’s Wort is not a 'mood booster.' It’s a serotonin grenade. I’ve seen three people in my yoga class go from zen to screaming in the parking lot after mixing it with SSRIs. If you’re going to self-medicate, at least have the decency to read the damn studies.
And yes, I’m mad. I’m always mad. But I’m mad because people die from this stuff. And no, I won’t stop yelling about it.
Lu Jelonek
Thank you for writing this. As a pharmacist in rural Ohio, I see this every day. Patients switch to generics because their insurance forces it, then come back confused because they’re suddenly dizzy or bloated. We don’t have time to explain every filler. But I always check the inactive ingredients list-lactose, FD&C dyes, titanium dioxide-and I’ll call the manufacturer if I need to. I wish more people knew this was a thing.
Also, the herbal supplement issue? I had a woman come in last week who was taking ashwagandha for 'stress' and didn’t realize it was lowering her blood pressure so much she was passing out in the shower. She thought it was 'just herbal.'
Education is the only antidote. Share this with your family. Print it. Tape it to the fridge.
Ademola Madehin
bro. i took a generic version of my antidepressant and i swear i felt like a ghost for 3 weeks. like my soul got replaced with a wet sock. i went to the dr and they were like 'maybe you’re just sad again' no. no i’m not. it was the fucking dye. i switched back and boom. i was human again. why does this even happen??
Jeffrey Frye
so like… the FDA says generics are bioequivalent but they don’t test for bioavailability differences in subpopulations? lol. what a joke. and don’t even get me started on how they let supplements with hidden sildenafil and steroids on the market. i mean, if you’re gonna scam people, at least make the product consistent. half these 'herbal' pills are just pharmaceuticals with a pine tree logo. also, acetaminophen is literally poison if you’re a light drinker. i’ve seen 4 cases of acute liver failure from people thinking 'i just took one extra tylenol.' it’s not a snack.
Andrea Di Candia
I’ve been thinking a lot about how we treat medicine like it’s a vending machine-you put in your insurance card, you get the pill, and you assume it’s perfectly calibrated for your body. But we’re all different. One person’s harmless filler is another person’s emergency room visit.
Maybe the real problem isn’t the drugs-it’s the system that treats us like interchangeable parts. We’re not data points. We’re humans with allergies, metabolisms, trauma, and histories. And yet we’re expected to navigate this maze alone, with labels written in tiny font and pharmacists rushing to the next customer.
I wish we could have more conversations like this-not just about what’s in the pill, but why we’re so afraid to ask. Why do we feel guilty for needing the brand name? Why do we assume 'natural' is innocent? Maybe if we stopped seeing medicine as something you just take, and started seeing it as something you *negotiate* with… we’d all be safer.
Pankaj Chaudhary IPS
This is a vital post. In India, the issue is even more acute. Many patients buy medicines from street vendors without prescriptions. I’ve seen children given adult doses of paracetamol because the label was torn off. Herbal remedies are often mixed with corticosteroids-unmarked, untested, and deadly.
But here’s the truth: access is the problem. People don’t choose generics because they’re reckless-they choose them because they can’t afford the brand. The solution isn’t to shame them. It’s to demand better regulation, transparent labeling, and affordable access to safe medications-not just for the wealthy.
Let’s fix the system, not just warn people how to survive it.
Gray Dedoiko
i’ve been on levothyroxine for 12 years. switched brands twice. first time i felt like i was underwater. second time i got panic attacks for no reason. i started asking for the exact brand every time. my pharmacist now calls me 'the thyroid lady.' i don’t care. i’d rather pay $20 extra than feel like i’m dying every month. also, i stopped all supplements. too many variables. i’m not a lab rat.
Aurora Daisy
Oh look, another American melodrama about pills. In the UK, we don’t have this problem because we have a national health service that actually regulates these things. You Americans think your 'freedom' to buy whatever junk you want from the internet is a virtue. It’s not. It’s a public health disaster wrapped in a 'self-care' bow.
And don’t even get me started on 'natural' supplements. If you’re going to swallow something that’s not regulated, at least have the decency to admit you’re gambling with your liver. But no-you’ll call it 'holistic' and blame your 'toxic workplace' for the migraines.
Just take your bloody prescription and stop pretending you’re a wellness influencer.
Steven Mayer
The pharmacokinetic variability between generic formulations of NTI drugs is statistically significant in 12–18% of cases, particularly for levothyroxine and phenytoin. The FDA’s bioequivalence threshold of 80–125% AUC and Cmax is insufficient for drugs with narrow therapeutic windows. The clinical implications are underreported due to confounding by indication and lack of longitudinal pharmacovigilance.
Furthermore, the absence of standardized inactive ingredient disclosure in consumer-facing labeling constitutes a regulatory gap in pharmacogenomic safety. The current OTC supplement market operates under DSHEA 1994, which explicitly prohibits pre-market safety evaluation. This creates a structural vulnerability in public health surveillance.
Recommendation: Implement mandatory barcoded inactive ingredient tracking at point-of-sale and require prescriber consent for generic substitution of NTI agents.
Charles Barry
Let me guess-this was written by a Big Pharma shill. You know what they don’t tell you? The FDA approves generics based on data from the brand-name companies themselves. Same labs. Same data. Same bribes.
And don’t tell me about 'fillers.' That’s a distraction. The real issue? The active ingredient isn’t even the same. I’ve had my own bloodwork done-different batches of the same generic have 15–20% variation in potency. The FDA doesn’t test for that. They just trust the manufacturer’s word.
And supplements? Of course they’re laced with drugs. Why? Because the FDA is asleep at the wheel. But here’s the real conspiracy: they don’t want you to know you can get the same effect from a $5 pill you buy off the street. They want you hooked on $150/month prescriptions.
Don’t be fooled. This isn’t about safety. It’s about profit.
Sidra Khan
i read this whole thing and then took 3 ibuprofen and a gummy vitamin. if i die, at least i died happy. 🍬💊💀
suhani mathur
As someone who grew up in a household where 'herbal tea' meant 'magic cure for everything,' I get it. My grandma swore ginger would cure her diabetes. She died of a stroke at 72. The ginger didn’t kill her-but the fact that she stopped her metformin for it? That did.
Don’t shame people for trying to heal themselves. But please, for the love of all that’s holy, tell your doctor you’re taking turmeric. Even if you think it’s 'just a spice.'
Also, if you’re taking St. John’s Wort and birth control? You’re not being 'natural.' You’re being a walking accident waiting to happen. I’ve seen three unplanned pregnancies because of this. Please. Just. Talk. To. Someone.
Joseph Manuel
The assertion that inactive ingredients are responsible for clinically significant adverse reactions in the majority of patients who report intolerance to generics is not supported by robust epidemiological data. While individual case reports exist, population-level studies indicate that the incidence of true hypersensitivity to excipients such as lactose is less than 0.5%. The perception of differential efficacy is more likely attributable to the nocebo effect, confirmation bias, and inadequate patient education.
Furthermore, the regulatory framework governing generic drug approval in the United States is among the most rigorous globally. The FDA requires demonstration of bioequivalence under fasted and fed conditions, with a 90% confidence interval for Cmax and AUC within 80–125%. This standard is scientifically validated and clinically protective.
While patient autonomy and informed consent are paramount, the dissemination of anecdotal narratives as medical fact risks eroding trust in evidence-based therapeutics and incentivizing unnecessary cost burdens on the healthcare system.