Drug Interaction Checker
Check for Medication Interactions
Enter two medications to see if they interact pharmacokinetically (how the body processes them) or pharmacodynamically (how they affect the body)
When you take more than one medication, your body doesn’t just treat them as separate things. They talk to each other-sometimes helpfully, sometimes dangerously. Two main ways this happens are called pharmacokinetic and pharmacodynamic interactions. Knowing the difference isn’t just for doctors and pharmacists. If you’re on multiple drugs-especially if you’re over 65-you need to understand how they might be working against each other.
What Pharmacokinetic Interactions Really Mean
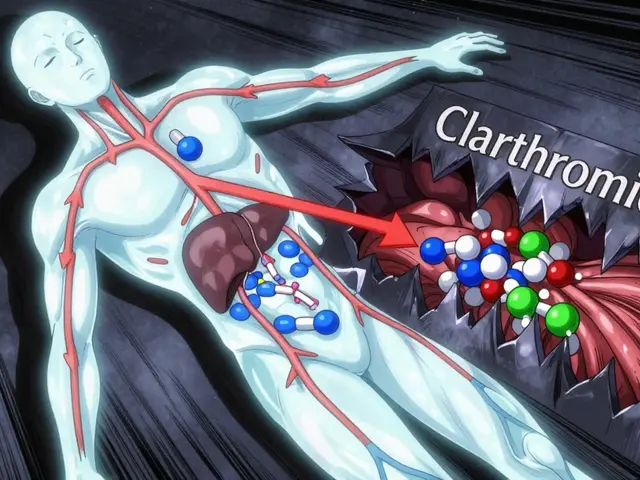
Pharmacokinetics, or PK, is what your body does to the drug. Think of it like a delivery system: how the drug gets in, moves around, gets broken down, and leaves your body. This process is called ADME: absorption, distribution, metabolism, and excretion. A common PK interaction happens when one drug blocks or speeds up how another is metabolized. The liver uses enzymes-mostly from the CYP450 family-to break down meds. CYP3A4 is the big one, handling about 75% of all drug metabolism. If you take clarithromycin (an antibiotic) with simvastatin (a cholesterol drug), clarithromycin shuts down CYP3A4. That means simvastatin builds up in your blood-up to 10 times higher than normal. That can cause muscle damage, even kidney failure. Another example: antacids like Tums or Maalox can stop antibiotics like ciprofloxacin from being absorbed. Studies show this cuts absorption by 75-90%. So if you take an antacid right before your antibiotic, it might not work at all. Warfarin, a blood thinner, is another classic case. It sticks tightly to proteins in your blood. If you add another drug like phenylbutazone, it kicks warfarin off those proteins. Suddenly, there’s 300% more free warfarin circulating. That’s why your INR can spike overnight-and why you need regular blood tests. These interactions are often predictable. If you know a drug affects CYP3A4 or P-glycoprotein (a transporter that moves drugs out of cells), you can guess what might happen. That’s why pharmacists check your meds every time you pick up a prescription. They’re looking for these red flags.What Pharmacodynamic Interactions Actually Do
Pharmacodynamics, or PD, is what the drug does to your body. It’s about the effect, not the amount. Two drugs can be at perfect levels in your blood, but still cause trouble if they hit the same target. The most dangerous PD interaction? Sildenafil (Viagra) with nitrates (like nitroglycerin for angina). Neither drug is toxic alone. But together, they massively drop your blood pressure-sometimes to deadly levels. That’s because both relax blood vessels. One dose of sildenafil plus a nitrate can send you to the ER. Another example: mixing SSRIs (like sertraline) with MAO inhibitors (like phenelzine). Both boost serotonin. Together, they can trigger serotonin syndrome: high fever, muscle rigidity, confusion, even death. That’s why doctors won’t let you switch from one to the other without a 2-week washout period. Additive effects are common too. Aspirin and warfarin both thin blood. Together, they don’t just add up-they multiply bleeding risk. That’s why many people on warfarin are told to avoid NSAIDs like ibuprofen. Then there’s antagonism. Naloxone (Narcan) is the classic. It blocks opioid receptors. If someone overdoses on heroin or oxycodone, naloxone doesn’t just reduce the effect-it reverses it. That’s PD in action: one drug directly cancels another’s effect at the receptor level. PD interactions are trickier. You can’t measure them with blood tests. Even if drug levels look normal, the combined effect can be severe. That’s why some combinations are simply banned-not because of levels, but because of what happens when they meet in your body.
Why the Difference Matters for Treatment
Here’s the key: PK interactions can often be fixed with a dose change. If clarithromycin raises simvastatin levels, drop the simvastatin from 40mg to 10mg. Done. You still get the benefit, without the risk. PD interactions? Not so easy. If two drugs act on the same receptor or pathway, lowering the dose usually doesn’t help. The problem isn’t the amount-it’s the combined effect. That’s why the FDA and NICE often say: don’t use them together. Period. This matters most with drugs that have a narrow therapeutic index-meaning the difference between a good dose and a toxic one is tiny. Warfarin, digoxin, phenytoin, lithium. For these, PK interactions are the main concern. But for antidepressants, opioids, and blood pressure meds, PD interactions are the silent killers. A 2022 study in the European Journal of Clinical Pharmacology found that 78% of serious CNS drug interactions were pharmacodynamic. That’s because the brain is full of overlapping systems-serotonin, dopamine, GABA, norepinephrine. Mess with one, and you might accidentally trigger another.How Clinicians Spot These Interactions Today
Most hospitals and pharmacies use electronic systems that flag interactions. Epic, Cerner, and other EHRs now check against databases with over 2,000 high-risk combinations. But they’re not perfect. They miss things-especially new combinations or subtle PD effects. That’s where pharmacists come in. In the UK, Specialist Pharmacy Service guidelines say: if you’re on five or more meds, you should have a medication review every year. For older adults, it’s even more critical. One in six people over 65 takes five or more drugs daily. That’s a recipe for hidden interactions. Therapeutic drug monitoring (TDM) helps with PK. Blood tests can tell you if your digoxin or lithium level is too high. But there’s no blood test for serotonin syndrome. You have to watch for symptoms: tremors, sweating, confusion, fast heart rate. New tools are emerging. AI models trained on real-world data now predict PD interactions with 89% accuracy-better than old rule-based systems. The FDA’s Sentinel Initiative has already flagged 17 new risky combos, including SGLT2 inhibitors (like dapagliflozin) with loop diuretics. Together, they can cause dangerous dehydration. That’s something no one thought about five years ago.
What You Can Do Right Now
You don’t need to memorize enzyme names or receptor types. But you can protect yourself:- Keep a list of every medication you take-prescription, OTC, supplements, even herbal teas. Include doses and why you take them.
- Ask your pharmacist: “Could any of these interact?” Don’t wait for them to ask you.
- If you start a new drug and feel weird-dizzy, nauseous, unusually tired-don’t ignore it. Call your doctor. It might not be the new drug. It might be how it’s talking to the old one.
- Don’t mix alcohol with sedatives, painkillers, or antidepressants. That’s a PD interaction waiting to happen.
- If you’re on warfarin, avoid sudden changes in vitamin K intake (like eating a lot of kale one week and none the next). That’s a PK + PD combo.
What’s Changing in 2026
The rules are getting stricter. The FDA now requires testing for 11 CYP enzymes and 8 transporters-not just the old 7. That means new drugs are being screened more thoroughly before they hit the market. Pharmacogenomics is also stepping in. If you have a CYP2D6 poor metabolizer gene, even a normal dose of codeine won’t work. But if you’re an ultra-rapid metabolizer, that same dose can turn into dangerous morphine levels. Testing for these genes is now part of standard care for some meds. And biologics-like immune checkpoint inhibitors for cancer-are creating new PD risks. Combine them with steroids or other immunosuppressants, and you might get severe infections or autoimmune damage. These interactions weren’t even on the radar a decade ago. The bottom line? Drug interactions aren’t just about pills. They’re about how your body’s systems talk to each other. PK is about the road the drug takes. PD is about what happens when it arrives. Knowing the difference helps you ask better questions. And in a world where polypharmacy is the norm-not the exception-that’s not just smart. It’s life-saving.Can pharmacokinetic interactions be detected with blood tests?
Yes, often. Blood tests called therapeutic drug monitoring (TDM) can measure drug levels in your bloodstream. This is commonly used for medications like warfarin, digoxin, phenytoin, and lithium. If a drug’s level is too high or too low, it may indicate a pharmacokinetic interaction-like a liver enzyme being blocked or sped up. But TDM doesn’t help with pharmacodynamic interactions, where drug levels are normal but the effect is too strong or too weak.
Are over-the-counter drugs safe to mix with prescriptions?
Not always. Many OTC meds cause serious interactions. For example, ibuprofen can increase bleeding risk when taken with warfarin or aspirin. Antacids can block antibiotics like ciprofloxacin. Even herbal supplements like St. John’s Wort can reduce the effectiveness of birth control pills, antidepressants, and heart meds by speeding up liver metabolism. Always check with a pharmacist before combining any OTC product with your prescription drugs.
Why do some drug interactions happen right away, while others take days?
Pharmacodynamic interactions often act immediately because they affect how your body responds to a drug at the receptor level-like how naloxone reverses an opioid overdose within minutes. Pharmacokinetic interactions usually take longer because they depend on changes in metabolism or absorption. For example, if a drug inhibits CYP3A4, it can take 3-5 days for the enzyme levels to drop enough to cause a buildup of the other drug. The body doesn’t react instantly-it needs time to adjust.
Can I reduce my risk of drug interactions by taking fewer medications?
Yes, absolutely. The more drugs you take, the higher your risk. Studies show that people taking five or more medications have a 50% chance of experiencing a significant interaction. A medication review with your doctor or pharmacist can help identify drugs that are no longer needed, duplicates, or those with high interaction potential. Sometimes, stopping one drug reduces the need for others-like lowering blood pressure without adding more pills.
Do pharmacokinetic interactions affect everyone the same way?
No. Genetics, age, liver and kidney function, and even diet play a role. For example, older adults often have slower metabolism, so they’re more sensitive to enzyme inhibitors. Some people have genetic variants that make them poor metabolizers of certain drugs-like CYP2D6 or CYP2C19. That means even a standard dose can become toxic. That’s why personalized medicine and pharmacogenomic testing are becoming more common in clinical practice.





shivani acharya
So let me get this straight - the FDA now tests for 11 CYP enzymes and 8 transporters, but my pharmacy still lets me buy St. John’s Wort next to my blood pressure meds like it’s a damn candy bar? 😒
And don’t even get me started on ‘natural supplements.’ That ‘herbal tea’ your cousin swears by? Probably shutting down your CYP3A4 while you sleep. Meanwhile, Big Pharma’s out here patenting the same damn mechanism they told you was ‘safe’ five years ago.
I’ve seen people on warfarin get sent home with a new antibiotic and zero warning. The system’s not broken - it’s designed to keep you dependent. You think they want you to understand ADME? Nah. They want you to keep showing up for refills.
And don’t even get me started on pharmacogenomics. They test your DNA, find you’re a poor CYP2D6 metabolizer, then charge you $800 for the report. Meanwhile, your doctor still prescribes codeine like it’s water. This isn’t medicine. It’s a pyramid scheme with stethoscopes.
They’ll give you a 20-page handout on ‘drug interactions’ but won’t tell you that your 80-year-old grandma’s 12 pills were prescribed by 7 different doctors who never talked to each other. That’s not negligence. That’s business.
Next time you see a ‘medication review,’ ask them: ‘Who’s actually accountable when this kills someone?’
And yes, I’ve seen people die from this. Not ‘rare cases.’ Not ‘anecdotes.’ Real people. With names. Who trusted the system.
So yeah. Keep taking your pills. Just know - you’re playing Russian roulette with a loaded gun labeled ‘prescription.’
Keith Helm
Pharmacokinetic interactions are quantifiable; pharmacodynamic interactions are not. This distinction is clinically fundamental.
Daphne Mallari - Tolentino
How quaint that laypersons are now being exhorted to understand ADME - as if pharmacology were a DIY home repair manual. The very notion that one ought to self-assess CYP450 interactions without formal training reveals a troubling erosion of professional authority.
Moreover, the conflation of therapeutic drug monitoring with comprehensive clinical judgment is not merely reductive - it is dangerously misleading. One does not diagnose serotonin syndrome with a blood test, nor does one manage polypharmacy by memorizing enzyme names.
Perhaps the real issue is not the drugs, but the commodification of health literacy - turning complex biomedical phenomena into TikTok soundbites for the algorithmically anxious.
Rob Sims
Oh wow, another ‘you need to know this’ article from someone who clearly thinks patients are just dumb animals who need to be told what to do.
Let me guess - you also think people should just ‘trust their doctor’ while their insurance denies the TDM test they need to even check if their lithium level is safe?
And you mention AI predicting PD interactions at 89% accuracy? Cool. So what? That means 11% of people still get screwed. And who pays when that’s you? Not the pharma rep who sold the combo.
Meanwhile, your ‘take a list’ advice? That’s what they tell you after you’ve already had a stroke from mixing warfarin and ibuprofen.
Don’t give me ‘what you can do.’ Tell me who’s gonna get fired when the system kills someone because they didn’t have the time, money, or access to do any of this.
arun mehta
This is such an important breakdown! 🙌
As someone from India where polypharmacy is rampant due to over-the-counter access and fragmented care, I’ve seen too many elders on 8+ meds with no coordination.
My aunt took ciprofloxacin with calcium tablets - and ended up with a UTI that didn’t clear for weeks. The pharmacist didn’t even ask what else she was taking.
Thank you for highlighting the difference between PK and PD - most people think ‘side effect’ means ‘bad reaction,’ not ‘drug talking to drug.’
Also, the part about SGLT2 + diuretics causing dehydration? That’s a silent killer. My uncle almost got hospitalized because he didn’t realize his ‘water pill’ and his new diabetes med were teaming up.
Keep sharing this. We need more clarity, not more pills. 💪❤️
Chiraghuddin Qureshi
From India, I can confirm - people here take antibiotics with tea, antacids with thyroid meds, and turmeric with blood thinners like it’s a cultural tradition 😅
My grandma swears by ‘herbal immunity boosters’ - turns out one of them inhibits CYP3A4 like a pro. She didn’t know, and no one asked.
Thank you for explaining PD vs PK so clearly. Now I can explain it to my cousins before they mix their antidepressants with ayurvedic ‘stress relievers.’ 🙏
Also - yes, the 2-week washout for MAOIs? That’s not a suggestion. That’s a life rule. I’ve seen what happens when people skip it.
Knowledge is the only real medicine here. 🌿
Kenji Gaerlan
bro why is this so long?? just say ‘don’t mix pills’ and be done lol
Oren Prettyman
The entire premise of this article is a dangerous oversimplification. You present pharmacokinetic and pharmacodynamic interactions as if they are mutually exclusive categories, when in reality, the distinction is often blurred - especially with polypharmacy in elderly populations.
For instance, the example of warfarin and phenylbutazone is cited as PK - but phenylbutazone also displaces warfarin from plasma proteins, which is a pharmacodynamic mechanism disguised as pharmacokinetic.
Moreover, the suggestion that dose reduction ‘fixes’ PK interactions ignores the nonlinear kinetics of many drugs - particularly those with narrow therapeutic indices. A 10mg reduction in simvastatin doesn’t linearly reduce risk; it may create a subtherapeutic window while leaving residual toxicity.
The FDA’s new testing requirements? A public relations gesture. Most drug interactions are identified *after* market approval, not before. The system is reactive, not proactive.
And AI models predicting PD interactions at 89% accuracy? That’s still a 1 in 8 chance of catastrophic failure. Would you trust a self-driving car with that failure rate?
What’s missing here is systemic critique - not patient education pamphlets.
Tatiana Bandurina
It’s fascinating how this article frames patient responsibility as the solution - ‘keep a list,’ ‘ask your pharmacist’ - while ignoring that most patients can’t afford to see a pharmacist, let alone get a medication review.
And yet, the same system that denies access to care blames you for not knowing that Tums block ciprofloxacin.
The real issue isn’t that people don’t understand ADME.
The real issue is that the healthcare system doesn’t care enough to make understanding unnecessary.
You don’t need a 15-sentence essay on CYP450 enzymes.
You need a single, coordinated provider who actually checks your meds.
But that’s expensive.
And profit-driven.
So we blame the patient instead.
Philip House
Look. I’ve read this entire thing. And I’ve seen the numbers. But here’s the truth nobody says: America doesn’t care if you live or die - as long as the bill gets paid.
They don’t want you to understand PK vs PD. They want you to think you’re in control. So they give you a checklist. A pamphlet. A ‘medication review’ that lasts 7 minutes.
Meanwhile, your doctor’s on a 12-patient-per-hour treadmill.
And your pharmacist? Probably got 30 scripts to fill before lunch.
This isn’t about education.
This is about survival in a broken machine.
And the machine? It’s rigged.
So yeah. Keep your list. Ask your pharmacist.
But don’t be surprised when the system eats you anyway.
Ryan Riesterer
The pharmacodynamic interactions described - particularly those involving receptor-level antagonism or additive effects - represent a significant clinical blind spot in current EHR systems. Most drug-interaction alerts are rule-based and calibrated for PK events, resulting in high false-positive rates and alert fatigue.
Conversely, PD interactions often lack quantifiable biomarkers, rendering them invisible to algorithmic flagging. The serotonin syndrome example is emblematic: no lab value correlates with onset, yet clinical consequences are severe and rapid.
Emerging AI models trained on longitudinal EHR and pharmacovigilance data show promise, but require integration with structured phenotyping - not just drug lists.
Until clinical decision support evolves beyond binary ‘high-risk’ flags to dynamic, context-aware risk stratification, PD interactions will remain underdetected and underappreciated in routine care.
Akriti Jain
Ohhh so now they’re telling us to ‘know your enzymes’? 😏
Meanwhile, your doctor prescribed you that new ‘miracle’ antidepressant… and your ‘natural’ sleep aid? Yeah, that’s the same CYP2D6 inhibitor they didn’t mention.
And the ‘pharmacogenomics’ testing? That’s just a way to upsell you another $500 test after you’ve already paid for the drug that doesn’t work.
They want you to think you’re smart for reading this… but you’re just being prepped for the next scam.
Who benefits when you’re confused? The pharmacy. The insurer. The drug company.
Not you.
And don’t even get me started on the ‘FDA testing’… they test the drugs, not the combo. So your 12-pill cocktail? Totally untested. 🤫
They’re not protecting you. They’re protecting their profits.
Wake up. 😈
Mike P
Man, this whole thing is wild. I’m 42, on 5 meds, and I didn’t know half this stuff.
But here’s the thing - I don’t have time to memorize CYP enzymes. I’ve got a kid, a job, and a mortgage.
So yeah, I took Tums with my antibiotic. Big deal? Maybe. But I didn’t know.
And now you’re telling me I’m at risk of kidney failure? Cool. Thanks for the guilt trip.
Why isn’t the system built to protect me instead of making me a pharmacist? Why don’t the pills come with a warning label that says ‘DO NOT MIX WITH THIS LIST’?
Why do I have to be the one to figure this out?
It’s not my job. It’s theirs.
And if they can’t make it simple, then they’re failing. Not me.
Jasmine Bryant
Hi! I just wanted to say thank you for this - I’m a nurse and I’ve seen so many patients confused about this exact thing.
One lady thought her ‘vitamin’ (St. John’s Wort) was fine with her antidepressant because it’s ‘natural.’ She ended up with serotonin syndrome.
Also - the part about warfarin and vitamin K? So many people don’t realize it’s not about ‘avoiding kale’ - it’s about consistency. Same amount, every day.
One typo I noticed: ‘P-glycoprotein’ is spelled right, but sometimes people confuse it with ‘P-glycoprotein’ - just a small thing!
Anyway, this is the kind of info we need more of. Clear, accurate, and not scary. 💙
shivani acharya
Oh, Jasmine, you sweet, naive angel.
You think a nurse saying ‘thank you’ changes anything?
That woman with serotonin syndrome? She’s still on the same meds. The hospital didn’t change the protocol. The pharmacist didn’t get fired. The rep who pushed the combo? Got a bonus.
You think ‘accuracy’ matters when the system is designed to ignore you?
Typo? Cute.
What about the typo that killed someone last week?
Keep smiling. Keep thanking. Keep believing the system cares.
Meanwhile, I’ll be over here watching the obituaries.
Rob Sims
And yet - the only thing that changed after that serotonin case? They added a pop-up alert in the EHR.
Which gets ignored 90% of the time because the nurse had 12 other alerts open.
So now we’ve got a ‘solution’ that doesn’t work.
And the patient? Still on the drugs.
Meanwhile, the company that made the SSRI? Still selling it.
They don’t want you to understand PK vs PD.
They just want you to keep clicking ‘accept.’