Psoriasis isn’t just a rash - it’s a full-body condition
When you see red, scaly patches on the skin, it’s easy to think of psoriasis as a simple skin problem. But it’s not. Psoriasis is a chronic autoimmune disease where the immune system mistakenly attacks healthy skin cells, speeding up their life cycle from 28 days to just 3-4 days. This causes thick, inflamed plaques to build up - often on elbows, knees, scalp, and lower back. It affects about 2-3% of people worldwide, with higher rates in Scandinavia and lower rates in East Asia. And while it can start at any age, it most commonly shows up between 15-25 or 50-60.
What makes psoriasis different from other skin conditions is how deeply it reaches. It’s not just about the surface. Up to 30% of people with psoriasis develop psoriatic arthritis, which causes joint pain, stiffness, and swelling. The inflammation doesn’t stop at the skin. People with psoriasis have a 58% higher risk of heart attack before age 50, and nearly half also have metabolic syndrome - high blood pressure, high cholesterol, and insulin resistance. Depression and anxiety are also twice as common in people with psoriasis compared to the general population. This isn’t just a skin issue. It’s a systemic condition that touches your heart, your joints, your mood, and your life.
Topical treatments are the first step - but they’re not enough for everyone
Most people start with creams and ointments. The most common first-line treatment is a combination of calcipotriol (a vitamin D analog) and betamethasone (a steroid). These are often sold as a single product to make application easier. For scalp psoriasis, foam versions work better than lotions. For the face or sensitive areas like the groin, doctors avoid strong steroids because they can thin the skin over time. Instead, they use milder vitamin D creams or calcineurin inhibitors.
But here’s the problem: sticking to a topical routine is hard. A 2023 survey of over 200 people on Reddit’s r/psoriasis found that 67% struggled with consistency. Why? The creams are messy. They stain clothes. They take time to rub in. Some burn or itch at first. And if you’re applying it twice a day, life gets in the way. That’s why simplifying the routine - like switching to once-daily application - can boost adherence by 40%, according to UCLA Health.
Topicals help, especially for mild cases. But if your plaques cover more than 5% of your body, or if they’re on your face, nails, or genitals, you’ll likely need more than creams. That’s when doctors move to the next level: light therapy or systemic treatments.
Phototherapy: Light as medicine
Narrowband UVB phototherapy is one of the most effective non-drug treatments. You sit in a light booth for a few minutes, 2-3 times a week, for about 8-12 weeks. It slows down the overactive skin cells and reduces inflammation. About 75% of people see major improvement after a full course. It’s safe for long-term use and doesn’t require injections or pills.
But there are downsides. You need to go to a clinic regularly. It’s not practical if you live far from a dermatology center. Home units exist - they cost between $2,500 and $5,000 upfront, plus $100 a month to maintain - but insurance doesn’t always cover them. PUVA, another light therapy that uses UVA light with a drug called psoralen, is less common now because it carries a higher risk of skin cancer over time.
For many, phototherapy is a bridge - a way to get control before moving to stronger drugs, or a way to avoid them altogether if their disease isn’t severe enough.
Systemic therapies: When the problem goes deeper
If your psoriasis is moderate to severe, or if it’s not responding to topicals or light therapy, you’ll likely be offered a systemic treatment. These are pills or injections that work inside your body to calm the immune system.
Traditional systemics include methotrexate, cyclosporine, and acitretin. Methotrexate is often used because it’s cheap and effective. But it can cause nausea, liver stress, and requires monthly blood tests. Cyclosporine works fast but can harm the kidneys if used longer than a year. Acitretin, a vitamin A derivative, is good for pustular psoriasis but can cause dry skin and is dangerous during pregnancy.
These older drugs still have a place, especially where cost is a barrier. But for many, the real game-changer has been biologics.

Biologics: Targeted treatment for targeted results
Biologics are drugs made from living cells that block specific parts of the immune system driving psoriasis. They’re not one-size-fits-all. There are different types:
- TNF-alpha inhibitors (like adalimumab and etanercept) - the first generation, still widely used
- IL-17 inhibitors (secukinumab, ixekizumab) - very fast-acting, often clear skin by 90%
- IL-23 inhibitors (guselkumab, tildrakizumab) - longest-lasting, some patients stay clear for over a year between doses
- IL-12/23 inhibitors (ustekinumab) - good balance of efficacy and safety
These aren’t cures, but they can get you to PASI 90 - meaning 90% of your plaques are gone. In clinical trials, secukinumab and guselkumab hit PASI 90 in more than 70% of patients after 16 weeks. That’s not just improvement. That’s near-complete clearance.
They’re given by injection, usually every few weeks or months. Most people learn to self-inject at home after one training session. Side effects are generally mild - injection site reactions, occasional colds. But you must be screened for tuberculosis and hepatitis before starting. And they’re expensive. Monthly costs range from $1,200 to $5,500, depending on insurance. Even with coverage, co-pays can hit $300 a month. That’s why 41% of patients delay or skip doses because of cost, according to the National Psoriasis Foundation.
Apremilast: An oral alternative to injections
If you hate needles but still need something stronger than topicals, apremilast might be your best bet. It’s a pill taken twice a day after a week-long ramp-up. It doesn’t suppress your whole immune system like biologics. Instead, it targets a specific enzyme inside cells called PDE4, which helps reduce inflammation.
It’s not as powerful as biologics - you’re more likely to get PASI 75 (75% improvement) than PASI 90. But it’s easier to take, doesn’t need blood tests, and has fewer infection risks. It’s also one of the few options that’s been shown to help with psoriatic arthritis. For people who want to avoid injections and aren’t looking for total clearance, apremilast offers a practical middle ground.
Comorbidities can’t be ignored
Doctors now know that treating psoriasis means treating the whole person. That’s why guidelines from the Primary Care Dermatology Society and the American Academy of Dermatology now require screening for other conditions at every visit.
Every person with psoriasis should have:
- Annual blood pressure checks
- Lipid panel (cholesterol and triglycerides)
- BMI tracking
- Depression and anxiety screening
- Joint pain assessment for psoriatic arthritis
Why? Because untreated psoriasis increases your risk of heart disease as much as diabetes does. And if you’re on a biologic, your immune system is suppressed - so catching an infection early matters. Your dermatologist isn’t just your skin doctor anymore. They’re part of your overall health team.
Real people, real struggles
On patient forums, the same stories come up again and again. People feel judged when they show up with flaky skin. They’re told to “just moisturize” or “stop stressing.” But psoriasis isn’t caused by stress - though stress can trigger flares. It’s not contagious. And it’s not a hygiene issue.
One woman in Bristol shared how she stopped wearing sleeveless tops after her first flare at 19. Ten years later, after starting secukinumab, she wore a tank top to the beach for the first time. “I didn’t realize how much I’d been holding back,” she said.
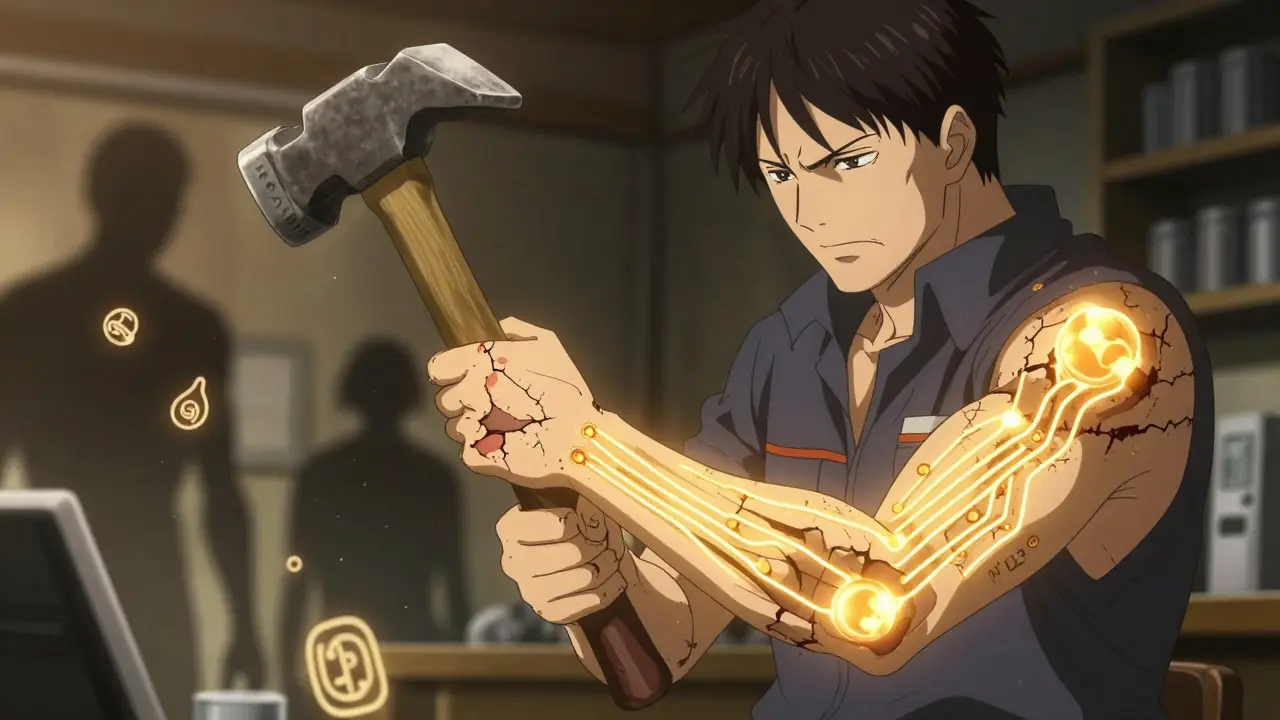
Another man, 52, stopped working because his hands were cracked and bleeding from palmoplantar pustulosis. After trying three oral drugs, he switched to guselkumab. Within three months, his palms were smooth. He went back to his workshop. He could hold tools again.
These aren’t rare successes. They’re the new normal - if you get the right treatment.
What’s next? Personalized care is coming
The future of psoriasis treatment isn’t just about better drugs - it’s about matching the right drug to the right person. Researchers are now looking at genetic markers to predict who will respond best to IL-17 inhibitors versus IL-23 blockers. New oral drugs like deucravacitinib (a TYK2 inhibitor) and RORγt inhibitors are showing promise in trials, with results matching biologics - but without injections.
Still, the biggest barrier isn’t science. It’s access. Only 25-30% of people with moderate-to-severe psoriasis get systemic treatment. In rural areas, there are 40% fewer dermatologists per square mile than in cities. Insurance hurdles, high costs, and lack of awareness keep people from getting the care they need.
Organizations like the National Psoriasis Foundation and the PCDS are pushing for better education, free support groups, and apps like MyPsoriasisTeam to help people track symptoms and treatments. These tools matter. Because managing psoriasis isn’t just about medicine. It’s about support, understanding, and not giving up.
What you can do today
- Moisturize daily - petrolatum-based products work best
- Take short, lukewarm showers with gentle cleansers
- Keep a symptom journal to spot triggers (stress, alcohol, injury, infection)
- Ask your doctor about screening for joint pain, blood pressure, and cholesterol
- If you’re not getting better with topicals, don’t wait - ask about phototherapy or systemic options
- Connect with others - support groups reduce isolation and improve outcomes
Psoriasis is lifelong. But it doesn’t have to control your life. With the right approach, most people can get to a point where they’re not just managing symptoms - they’re living well.
Is psoriasis curable?
No, psoriasis is not currently curable. It’s a chronic autoimmune condition, meaning the immune system keeps misfiring. But it is highly manageable. With modern treatments - especially biologics - many people achieve near-complete or complete clearance of their skin plaques. The goal isn’t a cure, it’s control: long-term remission, minimal symptoms, and a good quality of life.
Can psoriasis go away on its own?
Sometimes, yes - but rarely for long. Psoriasis often flares and then fades on its own, especially after infections or stress. But without treatment, it usually returns, often worse than before. Waiting for it to clear up naturally is risky. The longer inflammation goes untreated, the more likely you are to develop joint damage, heart disease, or depression. Treatment isn’t just about skin - it’s about protecting your whole body.
Are biologics safe for long-term use?
Biologics are generally safe for long-term use, but they do carry some risks. Because they suppress part of the immune system, you’re slightly more vulnerable to infections like tuberculosis or hepatitis. That’s why screening is required before starting. Serious side effects like cancer or nervous system disorders are rare. In real-world use over 15+ years, most patients tolerate biologics well. The benefits - clear skin, less joint pain, lower heart risk - usually outweigh the risks for moderate to severe cases.
Why do some people stop their psoriasis treatment?
The most common reasons are cost, side effects, and inconvenience. Biologics can cost over $1,000 a month even with insurance. Oral drugs like methotrexate cause nausea or fatigue. Injections require regular self-administration, which some find daunting. Others feel better after a few months and assume they don’t need the drug anymore - only to have a big flare later. Discontinuation rates are high - up to 50% within a year. Working with your doctor to find a sustainable plan is key.
Does diet affect psoriasis?
There’s no single psoriasis diet, but certain changes can help. Losing weight - even 5-10% - often improves symptoms because fat tissue produces inflammation. Cutting back on alcohol and processed sugars helps too. Some people benefit from reducing red meat and dairy, while others find omega-3s (from fish or flaxseed) reduce flare-ups. The key is to track your own triggers. What works for one person won’t work for another. A food journal can help you spot patterns.
Can psoriasis affect your mental health?
Absolutely. Studies show 17-37% of people with psoriasis have depression or anxiety - more than double the rate in the general population. The visible nature of the condition leads to shame, social isolation, and low self-esteem. Many avoid swimming, dating, or even going to work. Mental health isn’t a side effect - it’s part of the disease. That’s why screening for depression is now part of standard care. Talking to a counselor or joining a support group can be as important as your topical cream.
What’s the difference between psoriasis and eczema?
Psoriasis and eczema both cause red, itchy skin, but they’re very different. Psoriasis plaques are thicker, raised, and covered in silvery scales. They often appear on elbows, knees, scalp, and lower back. Eczema is usually more moist, oozing, and intensely itchy - often in the crooks of elbows or behind knees. Psoriasis is autoimmune; eczema is linked to skin barrier defects and allergies. Treatments differ too. Steroids help both, but biologics only work for psoriasis. A dermatologist can tell them apart with a simple exam.
Is psoriasis hereditary?
Yes, genetics play a big role. If one parent has psoriasis, you have about a 10% chance of getting it. If both parents have it, that jumps to 50%. But genes alone don’t cause it. You need a trigger - like stress, infection, injury, or certain medications. That’s why someone can carry the genes for decades and never develop psoriasis until something sets it off.




Stephen Craig
It's wild how the body turns on itself like this. Not just skin-deep, but a whole-system failure. We treat symptoms like they're isolated, but the immune system doesn't care about boundaries.
It's not a disease of the skin. It's a disease of connection.
Connor Hale
The part about biologics being expensive hits hard. I know someone who skipped doses for six months because of the co-pay. Then had a flare that landed them in the ER. The system fails people even when the science works.
Roshan Aryal
Western medicine keeps selling magic bullets while ignoring the real problem: our food, our stress, our toxic modern life. You think a $5000 injection fixes what processed sugar and cortisol did over decades? Pathetic. In India, we used turmeric paste and sunlight - and people lived longer without biologics.
Jack Wernet
This is one of the most comprehensive and clinically accurate summaries of psoriasis management I’ve encountered in a public forum. The integration of systemic comorbidities, adherence challenges, and therapeutic hierarchies reflects current dermatological consensus. Well-researched and respectfully presented.
Catherine HARDY
Have you ever wondered if Big Pharma is keeping psoriasis alive on purpose? I mean, biologics cost thousands a month, and they’re not a cure. What if they’re not trying to cure it? What if they need you dependent? Look at the timing - right after the FDA approved the first biologic, the number of diagnosed cases went up 300% in five years.
Vicki Yuan
I want to emphasize something crucial: the mental health component isn't secondary - it's foundational. When your skin visibly signals 'other,' society treats you like a problem, not a person. That shame compounds the inflammation. Healing requires both medication and validation. Thank you for including this.
Uzoamaka Nwankpa
I’ve had this since I was 17. No one ever believed me. My mom said I was just being dramatic. My boyfriend left me because he couldn’t ‘handle the flakes.’ I’ve cried in dermatology waiting rooms more times than I’ve had good days. I just wish someone had told me earlier: you’re not broken. You’re not ugly. You’re not contagious. You’re just sick. And you deserve care.
Chris Cantey
The real tragedy isn’t the plaques. It’s the silence. We’re taught to hide our bodies, to cover up, to pretend it’s not there. But what if we stopped apologizing for our skin? What if we stopped treating our bodies like enemies? The cure isn’t in a vial - it’s in radical self-acceptance.
Abhishek Mondal
While the article is superficially comprehensive, it fails to interrogate the epistemological framework underpinning Western dermatology: the reductionist paradigm that isolates skin from soul, symptom from system, and patient from power. The reliance on biologics - patent-protected, profit-driven, and culturally imperialistic - reflects a medical industrial complex that commodifies suffering. One must ask: who benefits when psoriasis is framed as a biological malfunction rather than a sociopolitical condition? The answer, as always, is not the patient.