When a doctor writes a prescription, they’re not just handing out a slip of paper-they’re taking on legal responsibility. And that responsibility has changed dramatically in the last decade, especially when it comes to generic drugs. Today, more than 90% of all prescriptions filled in the U.S. are for generics. That’s not just a trend-it’s the new normal. But behind that number is a growing legal minefield for physicians. Patients who suffer harm from generic medications can’t sue the drug maker. And that means the doctor who prescribed it might be the only one left standing in court.
Why Generic Drugs Changed Everything
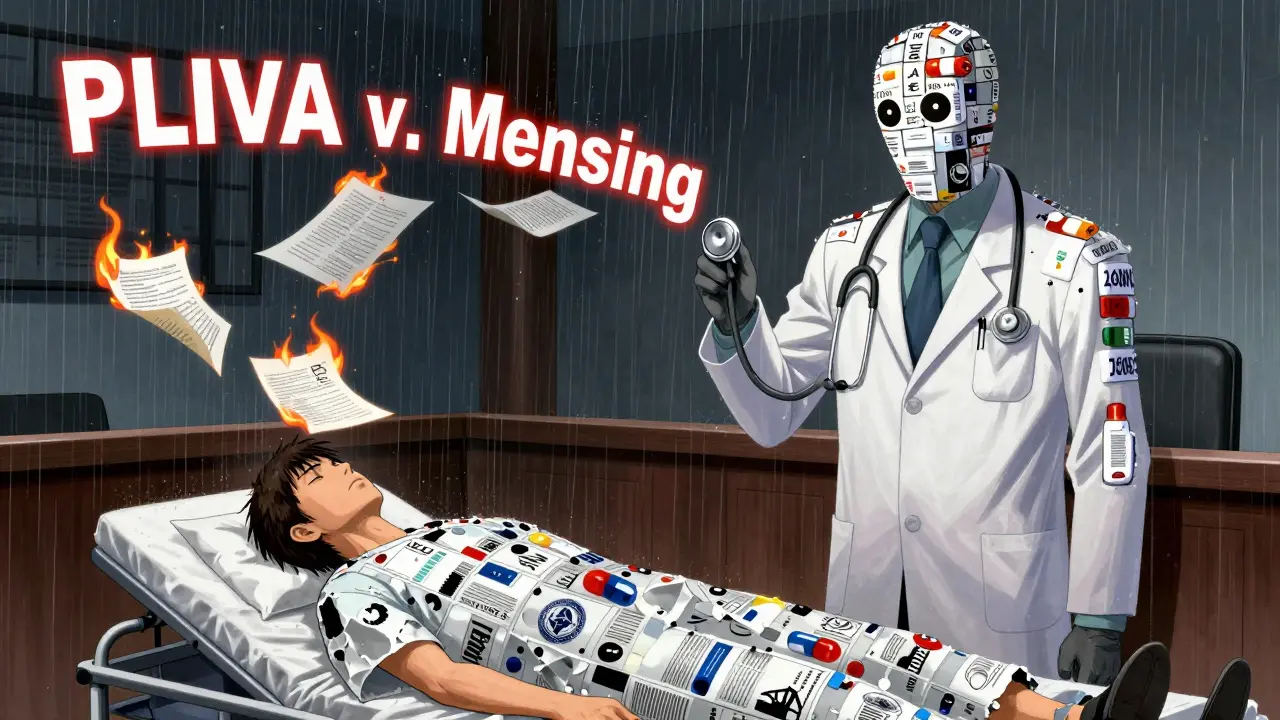
In 2011, the U.S. Supreme Court made a decision that reshaped medical liability forever. In PLIVA, Inc. v. Mensing, the Court ruled that generic drug manufacturers can’t be held liable for failing to update warning labels. Why? Because federal law says they must match the brand-name drug’s label exactly. They can’t change it on their own. That ruling was reinforced in 2013 with Mutual Pharmaceutical Co. v. Bartlett, where a woman lost 65% of her skin after taking generic sulindac. The Court said she couldn’t sue the manufacturer-even though the drug caused a rare, devastating reaction. The result? A legal gap. Patients hurt by generics have nowhere to turn. No lawsuit against the maker. No recall. No compensation from the company that produced the drug. So they turn to the person who wrote the prescription: the physician.What Makes a Doctor Liable?
To prove a doctor is legally responsible, a patient must show three things:- Duty: The doctor-patient relationship created a duty to provide safe care.
- Dereliction: The doctor failed to meet the standard of care-like not warning about known side effects.
- Direct cause: The medication directly caused the injury.
State Laws Make It Even More Complicated
Forty-nine states allow pharmacists to swap brand-name drugs for generics unless the doctor writes “dispense as written.” But here’s the catch: in 17 states, pharmacists aren’t required to tell the doctor they made the switch. That means a doctor could prescribe a brand-name drug, think they’re controlling the outcome, and then find out the patient got a generic version-without their knowledge. Some states try to fix this. In 32 states, pharmacists must notify the prescriber within 72 hours of substitution. But even that’s too late. Harm can happen in hours, not days. And then there’s the patchwork of court rulings. In Illinois, a court ruled in Guvenoz v. Target Corp. that generic manufacturers do have a duty to update labels if a drug is dangerously flawed. But in most other states, that’s not the case. So a doctor in Illinois faces different legal risks than one in Texas or Florida.
Defensive Prescribing Is Real
A 2022 survey of 1,200 physicians found that 68% feel more anxious about prescribing generics than they did five years ago. Nearly half admit they sometimes choose the more expensive brand-name drug-not because it’s better, but because they’re scared of being sued. One doctor in Massachusetts told a forum: “I now add written warnings to every prescription. It adds 15 to 20 minutes to every visit.” That’s not just time-it’s burnout. And it’s not just about paperwork. It’s about fear. The American College of Physicians recorded 47 malpractice claims tied to generic drugs between 2016 and 2021. Twelve of them ended in settlements averaging over $327,500. That’s not an outlier. It’s a pattern.What You Must Document
If you’re prescribing a drug that could cause drowsiness, dizziness, liver damage, or skin reactions, your documentation isn’t optional-it’s your shield. The Physicians’ Legal Handbook recommends using this exact language in your notes:“I have discussed potential side effects of [medication], including [specific side effects], and advised you to avoid [specific activities] while taking this medication.”Generic substitution counseling is now a mandatory field in Epic’s electronic health records system. If you don’t fill it out, the system won’t let you close the visit. That’s not bureaucracy-it’s liability prevention. Studies show physicians who document these conversations in detail reduce their risk of being sued by 58%. Insurance companies know this. And they’ve responded: premiums for doctors who routinely authorize substitutions without proper documentation have gone up by 7.3% on average.
Which Drugs Need Extra Caution?
Not all generics are equal. Some have a narrow therapeutic index-meaning the difference between a safe dose and a toxic one is tiny. These require extra care:- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin, carbamazepine, valproate (anti-seizure drugs)
- Lithium (mood stabilizer)
The Bigger Picture
The pharmaceutical industry spent over $14 million on lobbying since 2011 to protect generic manufacturers from liability. Meanwhile, Congress has considered bills like H.R. 958 to restore patient rights-but none have passed. The Supreme Court declined to review Colvin v. United States in 2022, keeping the preemption rule intact. But in March 2023, the 9th Circuit Court created a tiny crack in the wall: if a brand-name drug updates its warning label, and the generic doesn’t follow, the manufacturer can be sued. It’s a narrow exception, but it’s a start. The American Medical Association is now pushing for state laws that require pharmacists to notify doctors within 24 hours when they substitute a high-risk generic. Bills have been introduced in 18 states in 2023. If they pass, it could change how doctors manage risk.What You Can Do Today
You can’t control whether a patient gets a generic. You can’t control whether the manufacturer updates its label. But you can control your documentation, your communication, and your caution.- Always discuss side effects-out loud and in writing.
- Use “dispense as written” for drugs with narrow therapeutic windows.
- Document every conversation about substitution, even if the patient says they understand.
- Know your state’s substitution laws-some require notification, others don’t.
- Don’t assume a pharmacist will catch a dangerous interaction. You’re the last line of defense.
Can I be sued if a patient has a bad reaction to a generic drug I prescribed?
Yes. Since the Supreme Court’s 2011 and 2013 rulings, generic drug manufacturers can’t be held liable for failure-to-warn claims. That means patients who are harmed often sue the prescribing physician instead. Courts have upheld these lawsuits when the doctor failed to document proper counseling, didn’t warn about known risks, or ignored high-risk medication guidelines.
Do I have to use "dispense as written" on every prescription?
No-but you should use it for medications with narrow therapeutic indices like warfarin, levothyroxine, and certain anti-seizure drugs. In 32 states, this legally prevents substitution. For other drugs, it’s optional, but skipping it increases your liability risk, especially if the patient has a history of adverse reactions.
What if the pharmacist substitutes the drug without telling me?
In 17 U.S. states, pharmacists are not required to notify the prescribing physician about substitutions. That means you could prescribe a brand-name drug and the patient may get a generic version without your knowledge. This doesn’t absolve you of liability. You’re still responsible for ensuring the patient understands the risks of whatever medication they receive.
Can I be held liable if I prescribe a generic and the patient has an allergic reaction?
Yes-if you failed to ask about allergies, didn’t check for drug interactions, or didn’t document your discussion about potential side effects. The generic version must have the same active ingredient as the brand, so an allergy to one means an allergy to the other. Your liability depends on whether you met the standard of care, not whether the drug was generic or brand-name.
Has the number of lawsuits against doctors for generic drugs really increased?
Yes. According to the American Bar Association’s 2020 report, physician-targeted lawsuits involving generic drug injuries rose by 37% between 2014 and 2019. Legal experts predict a 45% increase by 2027 if current laws remain unchanged. Insurance premiums for primary care doctors have risen 22.7% since 2013, reflecting this growing risk.



Simon Critchley
Bro, this is the wild west of med-law. Generic manufacturers get a free pass? That’s not innovation-it’s corporate cowardice wrapped in federal preemption. I’ve seen patients turn into human pincushions from generic sulindac, and the pharma bros just shrug like it’s a beta test. Meanwhile, docs are left holding the bag with a scalpel and a subpoena. 😈
And don’t get me started on the ‘dispense as written’ loophole. I had a patient show up with a generic version of valproate that had 17% more bioavailability. She had a seizure in my waiting room. The pharmacist? ‘Oh, they’re bioequivalent.’ Yeah, right. Bioequivalent to what? A brick?
It’s not about liability-it’s about accountability. If the label’s wrong, someone needs to fix it. Not the doc. Not the pharmacist. The company that makes the damn thing. But nah. Congress is too busy lobbying for bigger tax breaks than actual patient safety.
And let’s be real: if you’re prescribing levothyroxine without documenting every damn word, you’re asking for a malpractice party. I’ve got a 3-page template now. My EHR even auto-generates a ‘you’re not dumb, but you’re still liable’ pop-up. It’s ridiculous. But necessary.
Meanwhile, my premiums went up 14% last year. Not because I’m bad at my job. Because the system is rigged. And we’re the collateral damage.
TL;DR: If you’re not using ‘dispense as written’ on narrow-therapeutic-index drugs, you’re playing Russian roulette with your license. And the gun’s loaded.
John McDonald
Man, I’ve been in this game for 22 years, and I’ve never seen a shift this drastic. Back in the day, we worried about brand-name side effects. Now? We’re auditing our own documentation like we’re preparing for trial tomorrow.
I’ve started printing out the FDA’s generic labeling guidelines and taping them to my desk. Not because I need to read them. Because I need to remind myself: ‘You’re the last line of defense.’
And honestly? I don’t blame pharmacists. They’re just doing their job. But the law needs to catch up. If a generic can’t update its label, then the prescriber should have the right to demand the brand. Period.
One of my patients got a generic version of warfarin. INR spiked to 8. She almost bled out. Turns out the generic had a different filler. Not the active ingredient-just the filler. And that’s what threw her off.
So now? I write ‘dispense as written’ on everything. Even if it’s just amoxicillin. Because I’m not risking my career on a 17-state loophole.
Chelsea Cook
Oh honey. You think this is bad? Wait till you see what happens when a patient sues you for prescribing a generic that’s ‘bioequivalent’ but somehow makes them cry uncontrollably for 3 days. 🤭
Let’s be real-the FDA’s ‘bioequivalence’ standard is basically ‘close enough for government work.’ Which, let’s be honest, is code for ‘we don’t care.’
I had a patient switch from brand to generic levothyroxine. She went from ‘I can run marathons’ to ‘I can’t get out of bed because my thyroid is on vacation.’
Turns out, different generics have different fillers. And fillers? They matter. Especially if you’re a 54-year-old woman with a gluten sensitivity and the generic used wheat starch.
So now I tell every patient: ‘If you feel weird after switching, come back. I’ll write ‘dispense as written.’ And if they argue? I say, ‘I’m not risking my license for a $20 savings.’
And yes, I’ve started charging extra for generic counseling. Because time is money. And my anxiety? That’s priceless.
Joshua Smith
This is such a messed-up system. I get that generics save money, but at what cost? I’ve been prescribing for 8 years, and I’ve never had a patient come back and say, ‘Hey, thanks for saving me $40 on this pill.’
But I’ve had 3 patients end up in the ER because they got a different generic version and had a reaction. One guy had a rash that looked like he’d been burned with a curling iron.
I started documenting every single conversation now. Even if they say ‘I’m fine.’ I write it down. ‘Patient stated understanding of side effects. Advised to avoid driving. No objections noted.’
It’s tedious. But I’d rather spend 10 extra minutes than lose my license.
Also-why does Epic force me to fill out a dropdown for ‘generic substitution counseling’? It’s not like there are 10 options. It’s ‘yes’ or ‘no.’ But if I don’t pick one? I can’t sign off. It’s like they know we’re all terrified.
Jessica Klaar
As someone who’s been on both sides of this-patient and caregiver-I just want to say this hits hard.
My mom had a stroke after taking a generic version of carbamazepine. The label said ‘may cause dizziness.’ It didn’t say ‘may cause loss of motor control, coma, or death.’
The pharmacist didn’t tell us it was switched. My mom’s doctor didn’t know. And the manufacturer? Silent.
We sued the doctor. It took 4 years. We settled for $120K. But we lost my mom’s independence. We lost her joy. We lost years of her life.
I don’t blame the doctor. I blame the system. But I also know-when you’re the one writing the script-you’re the only one who can speak up.
Please. Talk to your patients. Write it down. Even if they roll their eyes. Even if they say ‘I’m fine.’ Write it down.
Because sometimes, ‘I’m fine’ is the last thing they ever say.
Kathryn Lenn
So let me get this straight. Big Pharma lobbied Congress to shield themselves from liability… and now the doctor is the fall guy? 🤡
Classic. It’s always the doctor. Not the billion-dollar corporation. Not the FDA. Not the pharmacist who swaps pills like a blackjack dealer.
I bet if you dug into the lobbying records, you’d find that every single generic drug maker has a former FDA official on retainer. And guess who wrote the ‘bioequivalence’ guidelines?
It’s not a medical issue. It’s a financial one. And we’re the collateral. The system is designed to make doctors look like idiots so the real criminals walk free.
And don’t even get me started on ‘dispense as written.’ That’s not a medical decision-it’s a legal shield. Like putting a ‘Do Not Enter’ sign on your front door because you’re scared of the neighbor’s dog.
Wake up, people. This isn’t about patient safety. It’s about corporate liability. And we’re the suckers holding the bag.
Camille Hall
I love how we’re all scrambling to document everything, but no one’s talking about the real solution: fix the law.
I’ve been teaching residents for 15 years. I tell them: ‘Your notes are your armor.’ And they are. But armor doesn’t fix a broken system.
We need mandatory pharmacist-to-physician notification within 2 hours of substitution. Not 72. Not 24. 2.
And we need a federal override that allows generic manufacturers to update labels if new safety data emerges. The FDA has the power. They just won’t use it.
Meanwhile, I’ve started writing ‘dispense as written’ on *everything*. Even Tylenol. Because I’d rather look paranoid than be sued.
And yes, I’ve started asking patients: ‘Have you ever had a reaction to a generic before?’ It’s awkward. But it’s better than an ER visit.
Ritteka Goyal
OMG this is so true!! I am from India and we have so many generic drugs here and people get sick all the time!! My cousin took generic phenytoin and he had seizures and no one knew why!! The doctor said he prescribed the right thing but the pharmacist gave him a bad batch!! So now I tell everyone in my family: if you take generic, always check the manufacturer!! I even make them take a photo of the pill bottle!!
And in India, pharmacists change drugs without telling anyone!! No law!! No rules!! So doctors here are scared too!! We need a global law!!
Also, I think the FDA is just lazy!! They should test every single generic!! Not just ‘bioequivalent’!! That’s not good enough!! My aunt got liver damage from a generic and the company said ‘oops’ and kept selling!!
Please, doctors, please write everything!! Even if you think it’s dumb!! Write it!! Write it!! Write it!!
Monica Warnick
I just read this whole thing and I’m shaking. I mean-what if I’m the one who gets sued? What if I’m the one who prescribed the generic that made someone’s skin melt off? What if I’m the one who didn’t write ‘dispense as written’ because I was tired? What if I’m the one who forgot to document because I was running late?
I’ve been prescribed a generic before. I didn’t know it was generic. I got dizzy. I crashed my car. I was lucky I didn’t die.
Now I’m terrified to take any medication. I call my doctor every time I get a new script. I ask if it’s brand. I ask if it’s safe. I ask if it’s the same. I ask if the pharmacist told them.
And now I’m terrified to be a doctor.
Ashlyn Ellison
My doc started using ‘dispense as written’ on my levothyroxine after I told him I had a bad reaction. I didn’t even know that was a thing. Now I feel safer. Just saying.
Frank Baumann
Let me tell you about the time I prescribed a generic version of warfarin to a patient with atrial fibrillation. I didn’t write ‘dispense as written.’ I didn’t think it was necessary. The pharmacist swapped it. The patient’s INR went from 2.5 to 6.3. He bled into his brain. He’s paralyzed now.
I lost my license. My insurance dropped me. My wife left. My kids won’t speak to me.
I didn’t know. I didn’t mean to. But the law doesn’t care about intent.
Now I write ‘dispense as written’ on every script. Even if it’s Zyrtec. Even if it’s Advil. Even if it’s a vitamin.
I don’t care how long it takes. I don’t care if the patient rolls their eyes. I don’t care if the EHR is slow.
I’m not doing this again.