When someone falls asleep suddenly in the middle of a conversation, or their knees buckle out of nowhere during laughter, it’s not just being tired. It could be narcolepsy with cataplexy - a rare but deeply disruptive neurological disorder that’s often missed for years. This isn’t just about feeling sleepy. It’s about losing control of your body at the worst possible moments, and waking up to a life that feels like it’s slipping away. For many, it takes over a decade to get the right diagnosis. And when they finally do, the treatment path is just as complicated.
What Exactly Is Narcolepsy with Cataplexy?
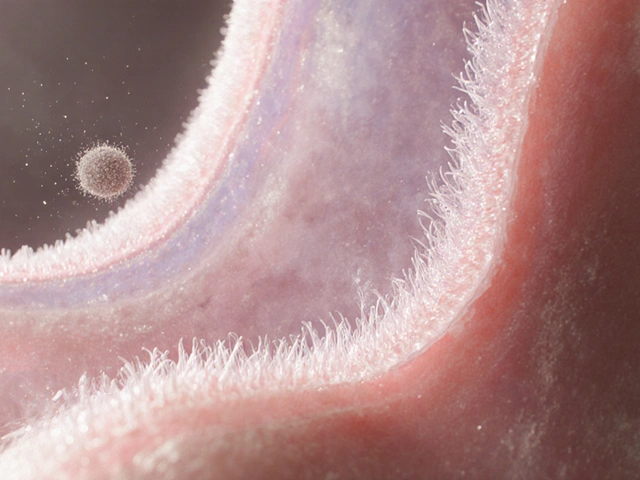
Narcolepsy with cataplexy, officially called narcolepsy type 1, is more than just extreme daytime sleepiness. It’s a brain disorder where the body loses its ability to regulate sleep and wake cycles properly. The key trigger? A shortage of hypocretin - a brain chemical that keeps you alert and controls muscle tone during emotions. Without it, your brain can’t tell the difference between being awake and falling asleep. The hallmark symptom is cataplexy: sudden muscle weakness triggered by strong emotions. It might start as a drooping eyelid when you laugh, or your jaw going slack during a joke. In severe cases, people collapse completely - legs giving out, head dropping - but stay wide awake. It’s terrifying if you don’t know what’s happening. Most people think it’s a seizure, a stroke, or just nerves. That’s why diagnosis is often delayed by 6 to 10 years. This isn’t rare. About 1 in every 2,000 people has it. And while it can start at any age, it usually shows up between 10 and 30. The genetic link is strong too - over 90% of people with this condition carry the HLA-DQB1*06:02 gene, compared to only 25% of the general population. But having the gene doesn’t mean you’ll get it. Something else - maybe an infection or immune reaction - triggers the destruction of the hypocretin-producing neurons in the brain.How Is It Diagnosed?
Getting diagnosed isn’t just a quick doctor’s visit. It’s a multi-step process that can take months and involves specialized testing. First, doctors look at your sleep history. Tools like the Epworth Sleepiness Scale help measure how sleepy you are during the day. If you score above 10, it’s a red flag. Then comes the sleep log - you record your sleep and wake times for at least a week. This helps rule out simple sleep deprivation. The next step is an overnight sleep study, called polysomnography (PSG). You’re hooked up to sensors that track brain waves, eye movements, heart rate, and muscle activity. This checks for other sleep disorders like sleep apnea. If you’re falling asleep too fast during the night or entering REM sleep too early, that’s a clue. The real test, though, is the Multiple Sleep Latency Test (MSLT). This happens the next day. You’re given four or five chances to nap, each two hours apart. Each nap lasts 20 minutes. If you fall asleep in under 8 minutes on average, and have at least two REM periods during those naps, it’s strong evidence of narcolepsy. But here’s the catch: MSLT isn’t perfect. Sleep deprivation, medications, or even stress can throw off the results. About 5 to 10% of people get false positives. There’s another way - and it’s more accurate. A spinal tap to measure hypocretin levels in your cerebrospinal fluid (CSF). If your levels are 110 pg/mL or lower, you almost certainly have narcolepsy type 1. This test is 98% sensitive and 99% specific. But it’s invasive. Lumbar punctures can cause headaches, and not every clinic offers them. Still, experts say if cataplexy is clear and the CSF test is positive, you might not even need the MSLT.Why Do People Get Misdiagnosed?
Most patients are misdiagnosed for years. Why? Because the symptoms look like other things. Cataplexy feels like fainting, dizziness, or panic attacks. Excessive daytime sleepiness gets written off as depression, laziness, or burnout. One survey of over 1,200 patients found that 68% were first told they had anxiety or depression. Another 15% were told they had sleep apnea. Even doctors can miss it. A 2022 Narcolepsy Network survey found that 79% of patients struggled to describe their cataplexy episodes. Some thought they were just “weak” or “shaky.” Others didn’t realize it was abnormal - until they collapsed at work or nearly got into a car accident. And there’s another problem: access. Only about 40% of U.S. sleep centers can properly run an MSLT. In rural areas, patients might drive hours just to get tested. That delay means years of untreated symptoms, lost jobs, failed relationships, and growing fear.
What Is Sodium Oxybate?
Sodium oxybate - sold under brand names like Xyrem and Xywav - is the only medication approved specifically to treat both cataplexy and excessive daytime sleepiness in narcolepsy type 1. It’s not a stimulant. It’s not an antidepressant. It’s a synthetic form of gamma-hydroxybutyrate (GHB), a naturally occurring brain chemical that helps regulate deep sleep. When taken at night, sodium oxybate helps patients get better quality sleep. It increases deep slow-wave sleep and reduces nighttime awakenings. The result? Less daytime sleepiness. But its real superpower is stopping cataplexy. Studies show it cuts cataplexy attacks by 75 to 90%. For many, it’s life-changing. The catch? It’s not simple to use. You have to take it twice a night - once at bedtime, and again 2.5 to 4 hours later. That means waking up in the middle of the night to drink a liquid that tastes like saltwater. Many patients say this is the hardest part. One study found 65% of users struggle with the midnight dose. Some fall back asleep and forget. Others can’t tolerate the nausea or dizziness. Xywav, introduced in 2020, is a newer version with less sodium. That helps people with high blood pressure or heart conditions. But the dosing schedule is still the same.How Is It Prescribed?
Sodium oxybate isn’t something your local pharmacy can fill. It’s tightly controlled because GHB has been used as a date-rape drug. That’s why every prescription goes through the Xyrem/Xywav REMS program - a national safety system. Doctors must complete a 60-minute training to prescribe it. Pharmacies must be specially certified. And patients must enroll in the program. No substitutions. No refills without re-certification. This adds layers of bureaucracy that delay treatment. Dosing starts low - usually 4.5 grams per night - and increases slowly over weeks. Most people need 2 to 3 months to reach their optimal dose. Side effects are common: nausea (38%), dizziness (29%), headaches, and sometimes bedwetting (12%). But for most, the benefits outweigh the downsides.Cost and Access Barriers
This treatment isn’t cheap. Before insurance, a month’s supply of Xyrem can cost $10,000 to $15,000. Even with insurance, patients often face prior authorization denials. A 2022 survey found 28% of patients had at least one claim rejected. Some wait months just to get approval. Insurance coverage varies wildly. Some plans cover it fully. Others require trial of other drugs first - like modafinil or pitolisant - even though those don’t treat cataplexy as well. In the U.S., only 45% of eligible patients actually get sodium oxybate, mostly because of cost and access. And yet, it’s the most prescribed treatment for this condition. In 2022, it made up 65% of all narcolepsy medication sales in the U.S. That’s because nothing else works as well for cataplexy.