When you’re pregnant and managing a mental health condition, the question isn’t just whether to take medication-it’s how to decide, with confidence, what’s best for you and your baby. Too many people are left guessing, scared of side effects, or pressured to stop meds cold turkey. But here’s the truth: there’s no risk-free choice. The real goal isn’t to avoid all medication-it’s to make a decision that’s informed, personal, and supported.
Why Shared Decision-Making Matters More Than Ever
Shared decision-making isn’t just a buzzword. It’s the standard of care. In 2023, the American College of Obstetricians and Gynecologists (ACOG) made it clear: if you’re pregnant and taking psychiatric medication, your provider should sit down with you-not tell you what to do, but walk through the risks and benefits side by side. This isn’t about being passive. It’s about being empowered. Why does this matter? Because untreated depression, anxiety, or bipolar disorder during pregnancy carries real dangers. Studies show a 20% higher risk of maternal suicide. Preterm birth rates jump by 30-50% when mental illness goes unmanaged. And those aren’t abstract numbers-they’re lives. One mom in Bristol told her doctor she was terrified of SSRIs. She stopped her medication cold. Within six weeks, she was hospitalized for severe depression. Her baby was born at 34 weeks. She didn’t need to go through that.What Medications Are Actually Safe?
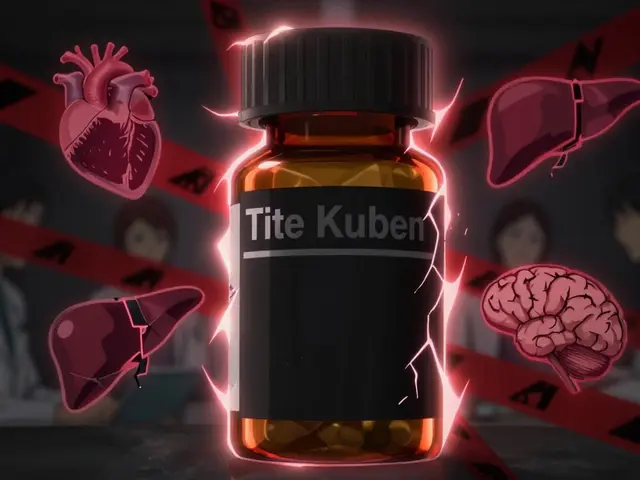
Not all psychiatric drugs are created equal. Some have decades of safety data. Others? Not so much. For depression and anxiety, SSRIs are the go-to. Sertraline (Zoloft), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac) are all considered first-line options. Why? Because large studies show they don’t increase the risk of major birth defects-except one. Paroxetine (Paxil) is linked to a small rise in heart defects: from about 8 in every 1,000 births to 10 in 1,000. That’s a real concern. So if you’re on paroxetine and planning pregnancy, switch before conception if you can. For bipolar disorder, lamotrigine is the safest bet. It doesn’t cause major birth defects. Lithium? It works-but your body changes during pregnancy. Your kidneys process it differently. That means levels can drop, leading to relapse-or rise, risking heart problems in the baby. Close monitoring is non-negotiable. Now, avoid valproic acid (Depakote) at all costs. It raises the risk of neural tube defects from 0.1% to 1-2%. That’s a 10- to 20-fold increase. It’s also linked to lower IQ and autism risk in exposed children. The American Psychiatric Association says it shouldn’t be used in women who could become pregnant. Period. Bupropion (Wellbutrin) carries a small risk of miscarriage and heart defects. Tricyclics like nortriptyline are older but still used when SSRIs fail. They’re not first-line, but they’re not dangerous either.Antipsychotics: What’s Known and What’s Not
If you’re managing psychosis or severe bipolar disorder, antipsychotics may be necessary. Typical ones like haloperidol (Haldol) and chlorpromazine (Thorazine) have been around for decades. Studies show no clear link to birth defects. That’s reassuring. But the newer atypicals-quetiapine, olanzapine, risperidone? We don’t have long-term data on kids exposed in utero. That’s why experts don’t recommend them as first choices unless absolutely needed. And even then, the goal is the lowest effective dose for the shortest time.
The Bigger Picture: Untreated Illness vs. Medication Risk
Here’s what most people don’t realize: the biggest risk often isn’t the pill. It’s the silence. A 2024 umbrella review in Nature found that many studies overstate medication risks because they don’t account for the illness itself. A pregnant woman with untreated depression has higher cortisol levels, worse nutrition, less prenatal care, and more stress-all of which hurt the baby. When researchers controlled for this, the difference in birth defects between medicated and unmedicated groups vanished. Dr. Lee Cohen, who runs the National Pregnancy Registry for Psychiatric Medications, puts it bluntly: “The risk of stopping treatment often outweighs the risk of continuing it.” For women with severe depression, relapse rates hit 80% if they stop meds during pregnancy. That’s not a small chance. That’s a near certainty.How Shared Decision-Making Actually Works
This isn’t a one-time chat. It’s a process. And it should start before you get pregnant. First, assess your risk. Have you had a previous episode? How long were you stable? The University of Washington’s Perinatal Psychiatry team says: if you’ve been symptom-free for at least three months before conception, your chance of relapse drops by 40%. That’s huge. Second, get the numbers. Don’t just hear “it’s safe.” Ask: “What’s the actual risk?” For example: “The chance of a heart defect with paroxetine is 10 in 1,000. The baseline risk is 8 in 1,000. So, 2 extra cases per 1,000 births.” That’s clearer than “slight risk.” Third, plan for the worst. What if your symptoms return? Who do you call? What’s your backup plan? Having this mapped out reduces panic later. ACOG’s Mental Health Medication Decision Aid gives you exact risk percentages for 24 medications. It’s updated quarterly using data from over 15,000 women enrolled in the National Pregnancy Registry. You should get a copy.
What Women Are Really Saying
A 2022 survey by Postpartum Support International found something shocking: 68% of women felt they weren’t properly informed before getting pregnant. And 42% stopped their meds on their own-because they were scared. In online communities like r/PostpartumDepression, 78% of posts describe pressure to quit meds. Many say they regretted it. One woman wrote: “I thought I was being brave. I wasn’t. I was just terrified. I ended up in the ER with suicidal thoughts at 28 weeks.” But those who used shared decision-making tools? They were 3.2 times more likely to stick with treatment. And at six weeks postpartum, their depression scores were 37% lower.What’s Changing in 2025
The field is moving fast. The National Pregnancy Registry is adding 12 new medications in 2024, including brexpiprazole, a newer antipsychotic with almost no pregnancy data. That’s good-because we need more info. By 2026, experts predict tools will use machine learning to give you personalized risk estimates-not just population averages. Imagine this: you’re 31, had two depressive episodes, took sertraline before pregnancy, and your BMI is 24. The system pulls data from 500 women just like you and says: “Your relapse risk without meds is 76%. Your baby’s risk of preterm birth with sertraline is 12%.” That’s not guesswork. That’s precision. And it’s not just science. It’s economics. Every $1 spent on structured shared decision-making saves $4.70 in later healthcare costs-fewer NICU stays, fewer emergency visits, fewer readmissions.What You Can Do Today
If you’re pregnant or planning to be:- Don’t stop your meds without talking to your provider. The risks of relapse are higher than most people think.
- Ask for the ACOG Mental Health Medication Decision Aid. It’s free and evidence-based.
- Find a perinatal psychiatrist. 87% of OB-GYNs now consult them regularly-ask yours if they do.
- Track your mood. Use the Edinburgh Postnatal Depression Scale (EPDS) every 4 weeks. It’s simple, free, and tells you when you need help.
- If you’re scared, you’re not alone. But silence won’t protect your baby. Informed action will.
There’s no perfect choice. But there is a right one-for you. And it starts with a conversation, not a fear.





Josh Potter
Bro, I stopped my Zoloft when I found out I was pregnant and now my wife’s in the psych ward. Don’t be that guy. Just don’t.
Jane Wei
my dr just told me to ‘try yoga’ and i cried in the parking lot
Salome Perez
Shared decision-making isn’t just ethical-it’s medically indispensable. The data is overwhelming: untreated maternal mental illness poses a far greater threat to fetal development than SSRIs. Paroxetine’s 10-in-1,000 risk? That’s statistically negligible compared to the 80% relapse rate when discontinuing. Empowerment isn’t about fear-it’s about evidence. And the ACOG decision aid? It’s the gold standard. If your provider won’t walk you through it, find one who will.
Steven Lavoie
As someone who’s navigated this while raising two kids, I can say with certainty: the fear of medication is often worse than the medication itself. I was terrified of sertraline too-until I realized my panic attacks were making me forget to eat, sleep, or go to prenatal appointments. The real danger isn’t the pill. It’s the silence. And the isolation. And the guilt that comes from thinking you’re failing your baby by staying alive.
My OB-GYN didn’t mention the National Pregnancy Registry. I had to find it myself. That’s a failure of the system. If you’re reading this and you’re pregnant or planning to be-ask for the decision aid. Demand it. Print it. Bring it to your appointment. You’re not being difficult-you’re being responsible.
And if your provider rolls their eyes? That’s not your fault. It’s theirs. There are perinatal psychiatrists who specialize in this. They exist. You just have to know to ask.
I also tracked my mood with the EPDS every four weeks. It saved me. When my score spiked at 18 at 24 weeks, I called my therapist before I even cried. That’s how you stay ahead of the curve.
There’s no perfect choice. But there’s a right one-and it’s the one you make with your eyes open, not your heart racing.
You’re not a bad mom for needing help. You’re a good mom for seeking it.
Victoria Rogers
They say SSRIs are safe but they never mention the 2023 FDA whistleblower report about hidden data on autism correlation. Big Pharma is pushing this agenda because they make billions. You think your baby’s safe? Wake up.
Jonathan Morris
They're hiding the truth. The FDA's own internal documents show that SSRIs alter fetal serotonin pathways permanently. They call it 'safe' because they don't track kids past age 5. What about the 12-year-olds with anxiety, ADHD, and sensory issues? Coincidence? Or corporate cover-up? I've seen the charts. The rise in neurodivergence tracks perfectly with SSRI use since 2005. This isn't medicine. It's chemical experimentation on unborn children.
CAROL MUTISO
Oh wow, so now we’re supposed to trust a government-funded registry run by the same people who told us thalidomide was ‘safe for morning sickness’? How quaint. I’ll take my chances with acupuncture and affirmations, thank you very much. At least then I’m not poisoning my child with corporate-approved antidepressants dressed up as ‘evidence-based care.’
Kaylee Esdale
you’re not broken for needing help
you’re brave for asking
your baby deserves a mama who’s okay
not a mama who’s quiet
Radhika M
I am from India and here doctors say stop all medicine. I had panic attacks. My baby was born healthy. But I cried every day for months. Please tell women: your mental health matters too.
Philippa Skiadopoulou
Accurate risk communication is the cornerstone of ethical obstetric care. The data on lamotrigine and sertraline is robust. The avoidance of valproate is non-negotiable. The challenge lies not in the science but in the dissemination of it. Clinicians must be trained to deliver these nuances without overwhelming patients. The ACOG tool is a vital step forward.
Meghan O'Shaughnessy
My OB didn’t even ask if I was on meds until I brought it up. I was 28 weeks. That’s not care. That’s negligence. If you’re pregnant and on psychiatric meds-don’t wait. Bring this article to your next appointment. Print it. Highlight it. Make them read it.
Pawan Chaudhary
God bless you for sharing this. I was scared too. Took sertraline through pregnancy. My daughter is 3 now-smart, happy, healthy. The meds didn’t hurt her. Not taking them almost broke me.
Naomi Lopez
How ironic that the same people who scream about ‘natural birth’ and ‘clean eating’ will tell you to stop your antidepressants like you’re some kind of herbivore in a wellness cult. You can’t ‘meditate away’ clinical depression. And if your provider thinks you can, you need a new one.