Medicare Part D isn’t just a drug benefit-it’s a carefully engineered economic system built to keep prescription costs down. And at the heart of that system? generic drugs. Since 2006, Part D has saved billions by steering beneficiaries toward cheaper, equally effective generics. But how exactly does it work? And why do some people still pay too much-even when generics are available?
How Part D Pushes Generics to the Front
Medicare Part D doesn’t hand out drugs directly. Instead, private insurers create plans with formularies-lists of covered medications-and organize them into tiers. Think of it like a pricing ladder. The lowest rung? Tier 1: Preferred Generics. These are the cheapest options, often with $0 to $10 copays for a 30-day supply. The goal? Make it easier and cheaper to pick a generic than a brand-name drug. In 2024, 87.3% of all Part D prescriptions were for generics. That’s up from just 55% when the program started. Why? Because the math works. A brand-name blood pressure pill might cost $45 a month. The generic version? $0. That’s not a coincidence-it’s by design. Plans put generics in Tier 1 because they know people will choose them. And when millions of seniors choose generics, the whole program saves money.The Cost Difference Isn’t Close
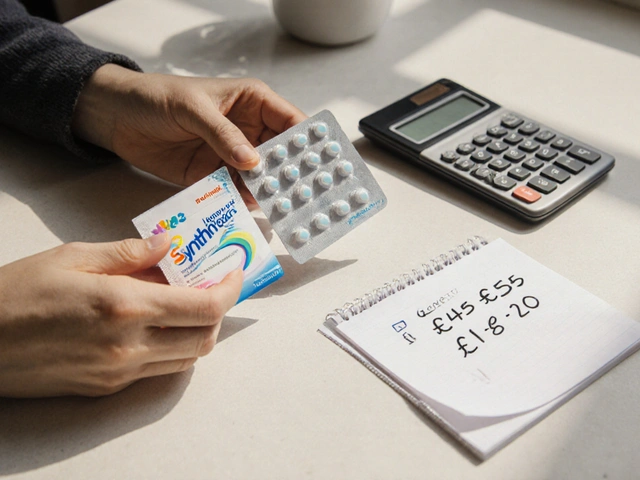
The gap between brand and generic prices is massive. In 2023, the average cost to Part D plans for a generic prescription was $18.75. For a brand-name drug? $156.42. That’s an 88% difference. Even when you factor in the 25% coinsurance beneficiaries pay during the initial coverage phase, the savings are huge. Take amlodipine, a common generic blood pressure med. On many plans, it costs $0 at preferred pharmacies. The brand-name version, Norvasc? $45 a month. That’s $540 a year just on one drug. Multiply that by the 51 million Medicare beneficiaries, and you’re talking about billions saved. But here’s the catch: not all generics are treated the same. Some specialty generics-like those for autoimmune diseases or mental health-get stuck in higher tiers. Even if they’re chemically identical to cheaper versions, they might cost $50 or more because the plan put them in Tier 3 or 4. That’s where beneficiaries get tripped up.How the ‘Donut Hole’ Changed Everything
The coverage gap-once called the “donut hole”-used to be a nightmare. Back in 2019, if you hit the gap, you paid 70% of the brand-name drug cost and 44% for generics. That meant people skipped doses or rationed meds to avoid bills. The Bipartisan Budget Act of 2018 changed that. Now, in the gap, you pay only 25% for both brand and generic drugs. That’s a game-changer. It means even if you hit the gap, you’re not punished for needing expensive meds. And since generics are cheaper to begin with, they’re even more attractive here.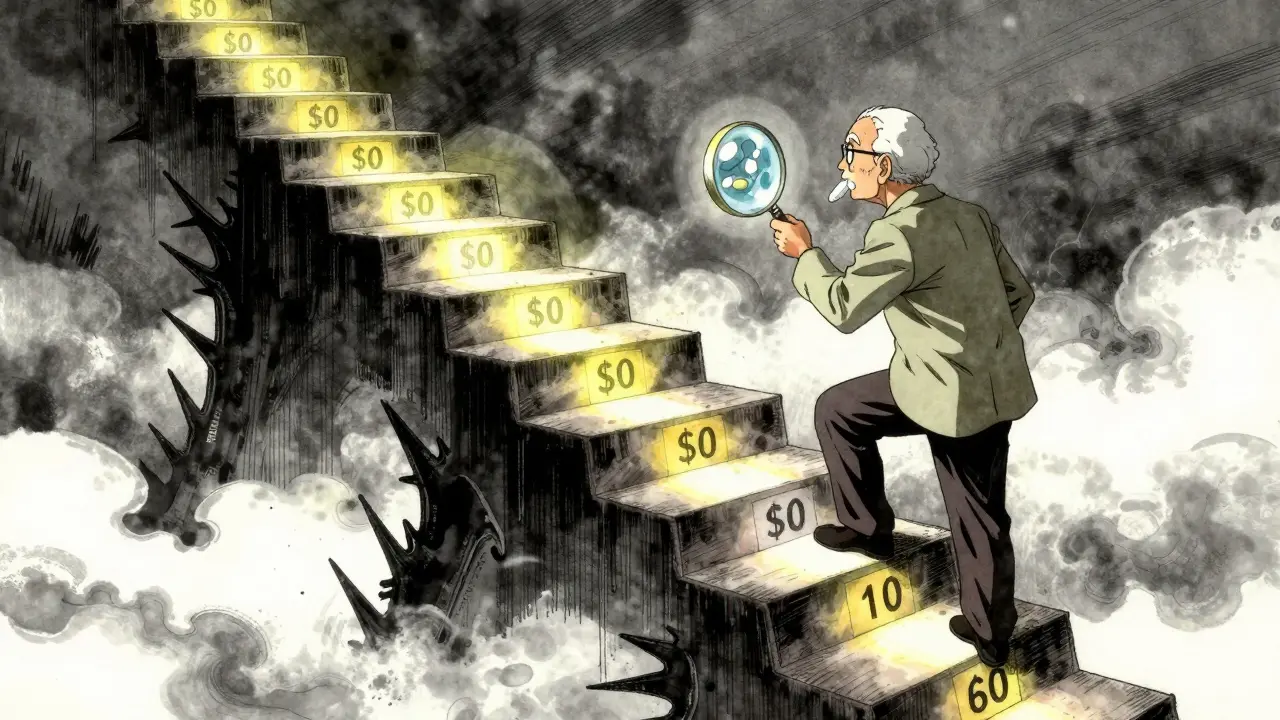
The ,000 Cap Is a Big Deal
Starting in 2025, Medicare Part D caps out-of-pocket drug spending at $2,000 a year. That’s huge. Before, some people with chronic conditions were paying thousands annually just for meds. Now, once you hit $2,000, the plan covers nearly everything. This change makes generics even more valuable. Why? Because the lower your drug costs early in the year, the faster you reach the cap. If you’re taking a $50 generic every month, you’ll hit the cap sooner than if you’re on a $150 brand-name drug. And once you’re past the cap, you pay just $4.15 for generics and $10.35 for brands.Who’s Winning? Who’s Losing?
The system works great for people who stick to generics. But it’s not perfect. Some beneficiaries get stuck with higher costs because their plan changes formularies mid-year. A generic that was $0 in January might jump to $30 in July. That’s legal-but it’s confusing. In 2023, 18.7% of complaints to CMS were about formulary changes that raised costs. Also, not all manufacturers play fair. Some brand-name companies offer coupons that can’t be used with Part D. So even if a coupon drops the brand-name drug to $10, you still pay $45 because the plan doesn’t accept it. That’s why some people end up paying more for the brand than the generic. Low-income beneficiaries are especially vulnerable. Even with generics, 32.1% of those in the lowest income bracket say they skip doses because of cost. That’s not because generics are expensive-it’s because they don’t understand how to pick the right plan.
How to Get the Best Deal on Generics
You don’t have to guess. Here’s how to make sure you’re getting the lowest price:- Use the Medicare Plan Finder during Annual Enrollment Period (October 15-December 7). Type in your exact medications-both brand and generic names.
- Look for plans with $0 copays on Tier 1 generics at your preferred pharmacy.
- Check if your drugs are on the formulary. Don’t assume your current plan will cover them next year.
- Ask your pharmacist if they’re automatically substituting generics. If you need the brand, ask your doctor to write “dispense as written.”
- If a generic causes side effects, request a “coverage determination.” CMS approves these requests 78.4% of the time.





Patrick Roth
Let me stop you right there - generics aren’t the hero here, they’re the scapegoat. The real savings come from insurers forcing patients into tiered formularies that penalize adherence. I’ve seen elderly neighbors skip doses because their ‘$0 generic’ was only $0 at one pharmacy 20 miles away. That’s not economics, that’s extortion dressed up as policy.
Jasmine Bryant
i just wanted to say i learned so much from this post!! i had no idea about the donut hole changes or the 2025 cap - i always thought generics were just cheaper but didn’t realize how much the system is designed around them. also, the pharmacist tip about automatic substitution? game changer. i’m gonna check my plan right now 😅
shivani acharya
Oh wow, so the government just turned us all into lab rats for Big Pharma’s profit margins? Generics? Sure. But did you know some of those ‘generic’ manufacturers are owned by the same companies that make the brand names? And the ‘$0 copay’? That’s only if you don’t mind waiting 3 weeks for your refill or if your pharmacy doesn’t ‘accidentally’ lose your script. This whole system is rigged. They want you to think you’re saving money while they just move the goalposts. And don’t get me started on the ‘manufacturer discounts’ - those are just accounting tricks to make the books look pretty before the next rate hike.
Hilary Miller
My abuela switched to amlodipine generics and now she has extra cash for tamales every Sunday. This system works if you know how to use it.
Margaret Khaemba
I love how this breaks down the real math behind it. My mom was on a brand-name antidepressant for years because she didn’t know the generic was the same - until I sat down with her and showed her the Plan Finder. She’s been on the generic for 18 months now and says she feels the same, just with more money for her weekly bingo. It’s wild how much info is out there if you just take 10 minutes to look.
Malik Ronquillo
So basically the government says ‘take the cheap pill’ and then acts surprised when people get sick because they’re too confused to figure out which one is actually covered this month? Wow. What a brilliant plan. I bet the lobbyists are throwing parties right now.
Daphne Mallari - Tolentino
The structural efficiency of Medicare Part D’s formulary architecture represents a paradigmatic shift in pharmaceutical cost containment. The deliberate tiering mechanism, calibrated to behavioral economics principles, incentivizes rational consumer choice through predictable copay differentials. One cannot overstate the macroeconomic implications of achieving 87.3% generic utilization - a figure that reflects not merely policy success, but a sophisticated alignment of market incentives and public health outcomes.
Sarvesh CK
It’s fascinating how this system, while imperfect, demonstrates what’s possible when policy is designed with both compassion and economic realism. The real tragedy isn’t the existence of tiered formularies - it’s that so many beneficiaries don’t know how to navigate them. I’ve spoken to retirees who’ve been on the same plan for 15 years, assuming their meds are still covered, only to discover their $0 generic now costs $40 because the plan changed mid-year. The burden shouldn’t be on the elderly to become pharmacoeconomists. What’s needed isn’t just better tools like the Plan Finder, but proactive outreach - perhaps through community centers, churches, or even postal mailers that don’t look like junk. The savings are real, but they’re meaningless if people don’t know how to claim them. And yes, the 2025 cap is monumental - it’s the first time in decades that the system has acknowledged that no one should have to choose between insulin and groceries. But let’s not pretend this is the end. We still have to fix the patchwork of pharmacy networks, the opaque formulary changes, and the predatory coupons that only benefit those who can afford to pay out-of-pocket. Generics are the engine, yes - but the whole vehicle needs better brakes, better maps, and a driver who actually cares.
Liberty C
Oh please. You think this is about ‘savings’? It’s about control. The system doesn’t want you to be healthy - it wants you to be compliant. Generics aren’t cheaper because they’re better - they’re cheaper because the pharmaceutical cartel has already extracted every dime it can from the brand-name version. And now? They’ve got you hooked on the ‘safe’ alternative while quietly raising the price of the next generation of ‘premium’ generics. You think your $0 amlodipine is free? It’s already been baked into your premiums. This isn’t economics. It’s psychological warfare disguised as benevolence.