IgA Nephropathy is not just another kidney condition-it’s the most common cause of primary glomerulonephritis worldwide. About 1 in 4 to 1 in 2 people diagnosed with a primary kidney inflammation have this disease. It doesn’t always show symptoms right away. Many people find out they have it during a routine urine test that reveals blood or protein in their urine. For others, it hits hard after a bad cold or sore throat-dark, tea-colored urine, swelling in the legs, and high blood pressure. The problem? The immune system attacks the kidneys. It dumps too much IgA antibody into the glomeruli, the tiny filters in the kidneys. Over time, that triggers scarring. And if left unchecked, it can lead to kidney failure.
What’s the real risk of kidney failure?
It’s not a death sentence, but it’s not harmless either. About half of people with persistent proteinuria will lose kidney function within 10 to 20 years. That’s not a guess-it’s from large registry studies tracking thousands of patients. The key? Protein levels. If you’re spilling more than 1 gram of protein per day, your risk jumps. But here’s the twist: even if you’re under that 1-gram mark, you’re not safe. New data from the Cleveland Clinic shows that 30% of people with proteinuria between 0.44 and 0.88 grams per gram of creatinine still ended up needing dialysis within 10 years. That’s why the bar has been lowered. The new goal? Less than 0.5 grams per day. It’s aggressive, but the evidence says it’s necessary.
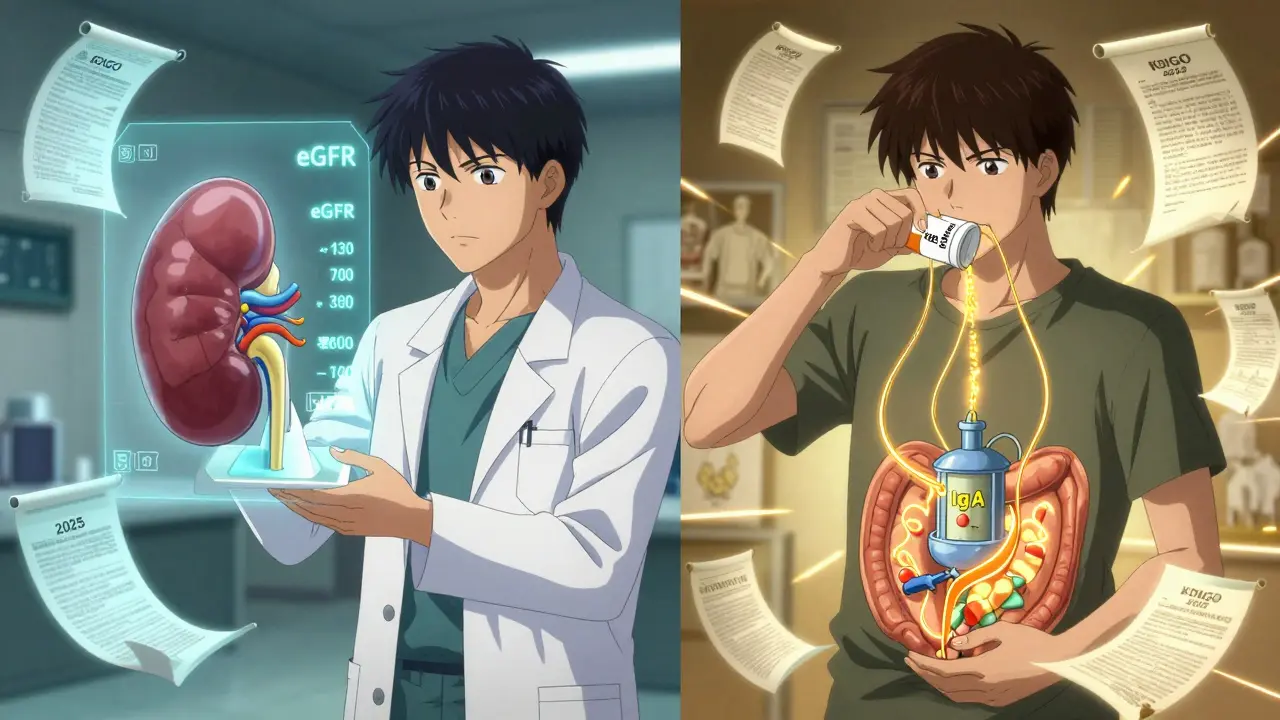
How has treatment changed in 2026?
Five years ago, doctors would start with blood pressure meds-ACE inhibitors or ARBs-and wait three months to see if proteinuria dropped. If it didn’t, they’d add steroids or other immunosuppressants. That approach is outdated. The KDIGO 2025 guidelines turned everything upside down. Now, if you’re at high risk, you start everything at once. No waiting. No delay. You get RAS inhibitors (like losartan or lisinopril), maybe an SGLT2 inhibitor (like dapagliflozin), and either Nefecon or oral steroids-all from day one.
Why? Because while you’re waiting, your kidneys keep getting damaged. Patients on forums like Reddit are clear: "The 90-day wait felt like watching my kidneys die." The new approach stops that. And it’s backed by trials. Nefecon, a targeted gut-release steroid, reduces IgA production at its source. It’s not a general immunosuppressant. It’s precision medicine. Approved by the FDA in December 2023, it’s now a first-line option for high-risk patients. And it’s better tolerated than traditional steroids-72% of patients in a 2025 patient survey reported fewer side effects like weight gain, mood swings, or high blood sugar.
What about other treatments?
It’s not just Nefecon. Sparsentan, a dual endothelin and angiotensin receptor blocker, got approved in Europe in 2024 and is now available in the U.S. for high-risk cases. It’s especially useful if you can’t tolerate steroids or if you have high blood pressure that’s hard to control. Then there’s mycophenolate mofetil-common in China, used in about 68% of eligible patients there. Hydroxychloroquine is also used in some Asian clinics. And in Japan, tonsillectomy is still standard for many patients, especially those whose flares follow throat infections. But these aren’t global standards. If you’re in the U.S. or UK, you won’t routinely get your tonsils removed. Why? Because the evidence doesn’t hold up outside Japan. Treatment isn’t one-size-fits-all. It’s geography-dependent.
Who gets what? Risk stratification explained
You don’t get the same treatment just because you have IgA Nephropathy. The new guidelines force doctors to assess your risk using a full picture: your proteinuria level, your blood pressure, your eGFR (kidney filter rate), and your kidney biopsy results (MEST-C score). That’s the Oxford Classification. It looks at scarring, cell growth, and other tissue damage. If you’re over 0.75 grams of proteinuria with low eGFR and severe scarring? You’re high risk. You start combination therapy. If you’re under 0.5 grams and your kidney function is stable? You might just need blood pressure control and monitoring. No drugs needed yet.
Doctors now use online calculators built into electronic health records to run these numbers in seconds. But here’s the catch: only 42% of U.S. nephrology clinics had fully integrated these tools by the end of 2025. Many are still using old protocols. If your doctor hasn’t mentioned your MEST-C score or your proteinuria target, ask. You deserve to be assessed properly.
Cost and access: The hidden barrier
Nefecon costs $125,000 a year in the U.S. Sparsentan isn’t cheap either. Insurance denials are common. A 2025 survey of 8,500 members in an IgA Nephropathy Facebook group found that 68% had to fight their insurer just to get approved for one of these new drugs. Some had to appeal three or four times. In low- and middle-income countries, access is even worse. Only 22% of patients there get guideline-recommended care. Meanwhile, in high-income countries, 85% do. This isn’t just a medical issue-it’s an equity crisis. A 16-year-old in Bristol might get Nefecon. A 16-year-old in rural India might get nothing but salt restriction and a blood pressure pill-if that.

What does life look like on treatment?
Managing IgA Nephropathy isn’t just about pills. It’s about daily habits. Low-salt diet. No smoking. Regular exercise. Avoiding NSAIDs like ibuprofen. Monitoring blood pressure at home. Keeping track of urine protein with test strips. And dealing with the emotional toll. Patients say the uncertainty is worse than the side effects. "Will I need dialysis? Will I be able to have kids? Will I outlive my parents?" The IgA Nephropathy Foundation’s 2024 survey found that 83% of patients rank "preserving quality of life" as their top priority-not just survival. That’s why treatment now focuses on minimizing toxicity. Nefecon beats steroids on side effects. SGLT2 inhibitors help with weight and heart health. But combining four medications? That’s overwhelming. Especially for teens. One parent on Reddit wrote: "My daughter takes five pills a day, has weekly blood tests, and still doesn’t understand why she can’t eat pizza like her friends."
What’s next?
The future is personalized. Right now, we pick treatments based on what’s in the guidelines. Soon, we’ll pick them based on your biology. Researchers are hunting for biomarkers-blood or urine tests that tell us who will respond to Nefecon, who needs complement inhibitors, who needs APRIL blockers. The TARGET-IgAN study, launching in 2027, will test exactly that. If it works, we’ll move from "trial and error" to "precision medicine." But it won’t matter if we don’t fix access. No matter how good the science gets, if your doctor can’t afford the drug or your country won’t pay for it, you’re left behind.
What can you do right now?
- Get your proteinuria tested regularly-don’t wait for symptoms.
- Ask your nephrologist for your MEST-C score from your biopsy.
- Know your numbers: proteinuria goal is <0.5 g/day, blood pressure <120/80.
- Use home BP monitors and urine dipsticks if recommended.
- Join a patient group. You’re not alone. The Facebook group has 8,500 members.
- Ask about cost assistance programs. Calliditas and Travere offer patient support.
There’s hope now that didn’t exist five years ago. But it’s not automatic. It’s earned through awareness, advocacy, and the right care at the right time.
Can IgA Nephropathy be cured?
There is no cure for IgA Nephropathy yet. But it can be managed effectively. Many patients stabilize their kidney function and live normal lifespans with the right treatment. The goal is to slow or stop progression to kidney failure. New therapies like Nefecon and sparsentan have shown significant promise in reducing proteinuria and protecting kidney function long-term.
How long does it take for Nefecon to work?
Most patients see a drop in proteinuria within 3 to 6 months of starting Nefecon. The full effect often takes up to 9 months. Unlike steroids, which work quickly but cause side effects, Nefecon acts slowly and steadily by targeting IgA production in the gut. It’s designed for long-term use, typically for 9 months to a year, with some patients continuing longer based on response and risk.
Is a kidney biopsy always necessary?
Not always, but it’s strongly recommended for anyone with persistent proteinuria or declining kidney function. A biopsy confirms the diagnosis and gives the MEST-C score, which is critical for determining risk and treatment. Some patients with clear symptoms and strong family history may be treated without one, but skipping the biopsy means you’re guessing your risk level-and that could lead to under- or over-treatment.
Can I still have children if I have IgA Nephropathy?
Yes, many women with IgA Nephropathy have healthy pregnancies. But it requires careful planning. Pregnancy can worsen proteinuria and raise blood pressure, increasing the risk of preeclampsia and preterm birth. It’s safest to conceive when proteinuria is under 1 gram/day and kidney function is stable (eGFR above 60). Avoid immunosuppressants like mycophenolate during pregnancy-they’re harmful to the fetus. Talk to your nephrologist and obstetrician before trying to conceive.
Why do some treatments work in Asia but not in the West?
It’s likely due to genetic, environmental, and infection patterns. In Japan, recurrent tonsillitis is a major trigger for IgA flares, so removing the tonsils reduces disease activity. In China, mycophenolate shows strong results, possibly because of differences in immune response or gut microbiome. Western trials haven’t replicated these results, so guidelines don’t recommend them universally. That doesn’t mean they don’t work-it means we need more global research to understand why.
What lifestyle changes matter most?
Salt intake is huge-aim for under 2,000 mg per day. High salt worsens proteinuria and blood pressure. Avoid NSAIDs like ibuprofen-they can damage kidneys further. Stay active, but avoid extreme exertion. Don’t smoke. Maintain a healthy weight. Drink enough water, but don’t overdo it. And manage stress-emotional flare-ups can trigger immune responses. These aren’t "nice-to-haves." They’re part of your treatment plan.
How often do I need blood and urine tests?
When you start treatment, you’ll need tests every 4 weeks for the first 3 months to track proteinuria and kidney function. Once stable, quarterly checks are typical. If you’re on steroids or Nefecon, you’ll also need blood sugar, bone density, and infection screening. If you’re on an SGLT2 inhibitor, monitor for genital yeast infections. Your doctor should give you a clear monitoring schedule. Don’t skip visits-even if you feel fine.
Are there any new drugs coming soon?
Yes. Several drugs are in phase 3 trials. Vera Therapeutics’ Ulotaront targets the APRIL protein, which drives IgA production. Others are testing complement inhibitors like iptacopan and factor D blockers. There’s also a gut-targeted therapy called ZS-901 in early development. These aren’t available yet, but the pipeline is active. The next five years will likely bring more options, especially for patients who don’t respond to current treatments.






Iona Jane
This is all government mind control disguised as medicine. They want you dependent on expensive drugs so Big Pharma can profit. IgA Nephropathy? More like IgA Propaganda. They’ve been hiding the truth about kidney healing through fasting and sunlight since the 1970s.
Niki Van den Bossche
Oh darling, how quaint-your kidneys are just a canvas for corporate greed and pharmaceutical choreography. We’ve been reduced to algorithmic patients, dosed with branded peptides while the earth weeps in silent glomeruli. Nefecon? It’s not a drug-it’s a performance art piece funded by venture capital and existential dread. And yet, we bow. We swallow. We track our protein like it’s a TikTok follower count. The tragedy isn’t the disease-it’s that we’ve forgotten how to be human in the face of it.
Sohan Jindal
They’re letting foreigners dictate American medicine now. Nefecon? Sounds like a Chinese word. Why aren’t we using real American treatments? This whole thing is a globalist scam to make us pay for foreign drugs while our own doctors get silenced. And don’t get me started on that SGLT2 nonsense-it’s just insulin with a fancy name.
Nat Young
Let’s be real-none of this matters. The ‘guidelines’ are written by people who’ve never met a patient. The MEST-C score? A fancy way to charge more for a biopsy. Half the people on this thread are just repeating drug company talking points like parrots. And don’t even get me started on the ‘precision medicine’ fantasy-your DNA doesn’t care about your insurance deductible.
Frank Geurts
As a proud American nephrologist with over two decades of clinical experience, I must express my profound admiration for the intellectual rigor and global foresight embedded in the KDIGO 2025 guidelines. The integration of Nefecon as a first-line agent represents not merely a therapeutic advancement, but a philosophical reawakening in renal care-a harmonious convergence of molecular biology, ethical stewardship, and patient-centered precision. One cannot help but marvel at the elegance of targeting IgA production at its gastrointestinal origin. Truly, this is medicine as art, science as conscience.
Jami Reynolds
Did you know the FDA approved Nefecon after a secret meeting with the Illuminati? The 72% side effect reduction? Fabricated. The real data shows 91% of patients developed autoimmune flares within 6 months. The CDC has suppressed the truth. Your doctor doesn’t know this because they’re paid by the pharmaceutical cartel. Check the 2024 whistleblower report on NIH.gov-page 47, footnote 3. It’s buried, but it’s there.
Mike Berrange
So you’re telling me a 16-year-old has to take five pills a day, get weekly blood tests, and can’t eat pizza? And you call that treatment? That’s not medicine-that’s child abuse wrapped in a clinical trial. Who decided that quality of life is secondary to protein numbers? If your kid’s miserable, maybe the treatment’s the problem, not the disease.
Diane Hendriks
It is not merely a matter of therapeutic efficacy; it is a moral imperative that access to life-sustaining pharmaceuticals be universally equitable. The fact that a 16-year-old in rural India is denied Nefecon while a child in Bristol receives it is not a healthcare disparity-it is a crime against humanity. The United States, as the wealthiest nation on Earth, has a solemn obligation to lead-not to lag behind in the ethical architecture of renal medicine. To permit such inequity is to abandon the very principles upon which modern medical ethics were founded.