More than 1 in 4 pregnant women take herbal supplements. Not because they’re reckless, but because they’re told it’s natural, gentle, and safe. The truth? It’s not that simple. While some herbs like ginger have solid evidence backing their use, others carry hidden risks - risks that aren’t listed on the label, aren’t studied in pregnant women, and aren’t always understood by the people selling them.
Why Herbal Supplements Are So Common in Pregnancy
Nausea hits 35% to 80% of pregnant women. Sleep disappears. Anxiety creeps in. And suddenly, the idea of popping a pill feels wrong. Herbal teas, capsules, and tinctures feel like a better choice - natural, gentle, maybe even traditional. In Catalonia, 48% of pregnant women used at least one herbal product. In some parts of Asia, that number jumps to 58%. In the U.S., it’s around 29%. These aren’t fringe habits. They’re mainstream. But here’s the problem: no one is checking what’s actually in those bottles. The FDA doesn’t require herbal supplements to prove safety or effectiveness before they hit the shelf. That means one brand’s ginger capsule might have 500 mg of active compound. Another’s might have 150 mg - or worse, it might have undeclared herbs, heavy metals, or even prescription drugs. A 2023 FDA review found 20% to 60% of herbal products had inconsistent ingredients or incorrect dosages.What’s Actually Safe? The Evidence on Top Herbs
Not all herbs are created equal. Some have been studied in pregnant women. Others haven’t been studied at all. Here’s what the data says:- Ginger (Zingiber officinale): This is the gold standard. Multiple studies, including a 2023 Cleveland Clinic review, show it reduces nausea and vomiting as effectively as some prescription anti-nausea meds - without the same side effects. Doses under 1,000 mg per day are considered safe. Most women use it in the first trimester, and it’s the most popular herbal remedy in pregnancy worldwide.
- Cranberry (Vaccinium macrocarpon): Used to prevent urinary tract infections (UTIs), which are common in pregnancy. Studies suggest it works, but not as reliably as antibiotics. And here’s the catch: some women report spotting in the second or third trimester after taking cranberry supplements. That’s not a minor side effect. It’s a red flag.
- Chamomile (Matricaria recutita): Often sipped for sleep or calm. Sounds harmless, right? But a 2023 review by the American Academy of Family Physicians flagged possible links to preterm birth, low birth weight, and even issues with fetal heart development. The evidence isn’t strong, but it’s enough to warrant caution.
The Dangerous Myths: Herbs That Can Hurt
Some herbs are marketed as “toning” or “preparing the body for labor.” That sounds empowering - until you realize what’s really happening.- Red raspberry leaf (Rubus idaeus): This is the most controversial. Many midwives and wellness influencers say it strengthens the uterus and shortens labor. But the American Academy of Family Physicians says it’s “likely unsafe” for labor induction. One study found women who took it in the third trimester had a higher rate of cesarean deliveries. Why? Because it can trigger contractions - and not always in a controlled, safe way. There’s no standard dose. One tea bag might be fine. Five might be dangerous.
- Rosemary (Rosmarinus officinalis): Used in cooking? Fine. Taken as a supplement? Possibly unsafe. Oral doses can stimulate the uterus. That’s why it’s flagged as risky, even though rosemary oil in lotions is considered low risk.
- Pennyroyal, blue cohosh, sage, black cohosh: These are outright dangerous. They’ve been linked to uterine contractions, fetal distress, and even miscarriage. Yet they’re still sold online as “natural labor inducers.”

Why the Evidence Is So Gaps
You’d think with millions of pregnant women using herbs, we’d know more. But here’s the truth: pregnant women are almost never included in clinical trials. Not because they’re ignored - because scientists are afraid of harming the baby. So we’re left with small studies, animal data, and anecdotal reports. The CDC says fewer than 10% of all medications approved since 1980 have enough data to say they’re safe in pregnancy. Herbal supplements? Almost none do. That’s not a gap. That’s a chasm. Even when studies exist, they’re messy. One study might use 1 gram of raspberry leaf. Another uses 2.5 grams. One brand uses dried leaves. Another uses extracts. You can’t compare them. You can’t trust them. And you can’t be sure what you’re actually taking.What Doctors Really Think
The American College of Obstetricians and Gynecologists (ACOG) says it plainly: “Do not take any herbal products without talking to your health-care provider first.” The Cleveland Clinic is even blunter: “People who are pregnant are encouraged to avoid most herbal supplements.” Why? Because the risks aren’t theoretical. In Spain, 42% of women started taking herbal products without telling their doctor. They got advice from family, Instagram, or Reddit. One woman in the study took cranberry and started spotting. Another took raspberry leaf and went into labor early. Neither knew it could happen. Doctors aren’t anti-natural. They’re pro-safe. And right now, “natural” doesn’t mean “safe.” It means “unknown.”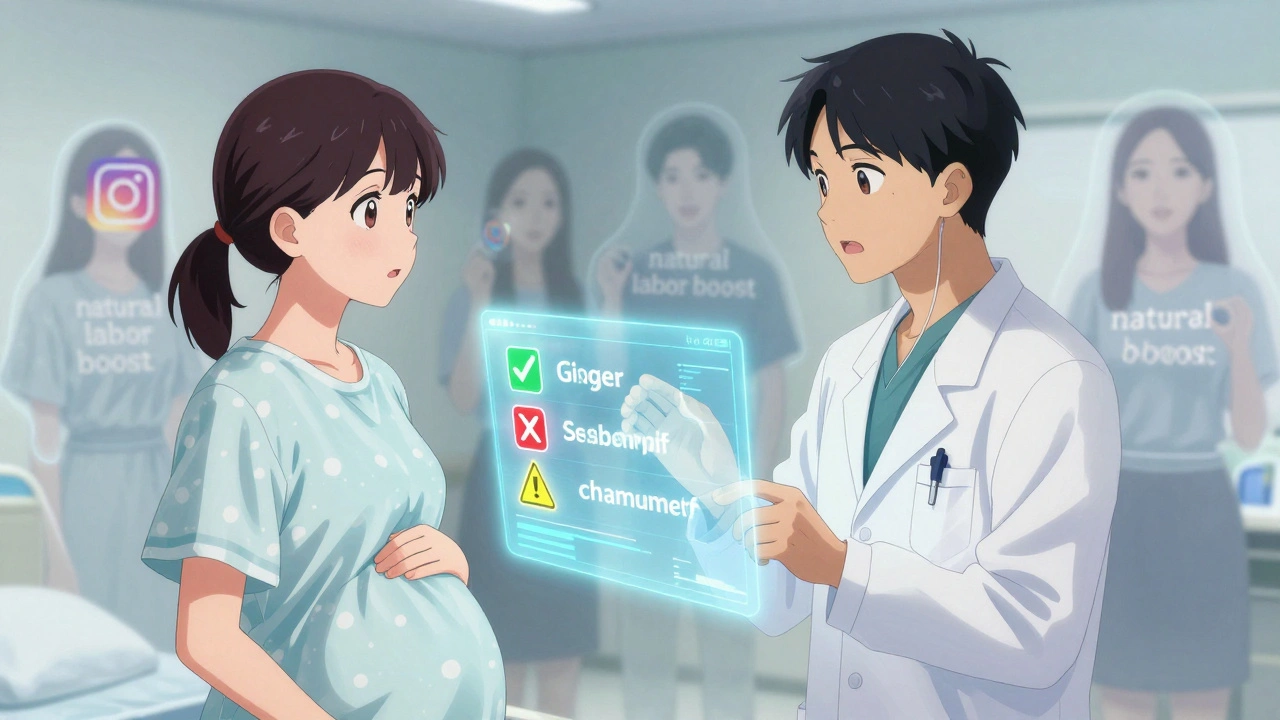
What You Should Do Instead
If you’re pregnant and thinking about herbs, here’s what to do:- Don’t guess. If you’re using something, tell your provider - even if it’s “just tea.”
- Only use ginger for nausea. It’s the only herb with consistent, strong evidence. Stick to 250-500 mg, 3-4 times a day. Ginger tea is fine too - just don’t drink 10 cups a day.
- Avoid anything labeled “labor-inducing” or “uterine-toning.” Those are red flags. There’s no safe way to induce labor with herbs.
- Check the label. Look for third-party testing (USP, NSF, or ConsumerLab). If it’s not there, don’t risk it.
- Ask about alternatives. For nausea: vitamin B6 or acupressure wristbands. For sleep: magnesium or cognitive behavioral therapy. For UTIs: cranberry juice (not supplements) and plenty of water.
The Bigger Picture
The herbal supplement industry is worth over $85 billion. A lot of that money comes from pregnant women looking for control, comfort, and safety. Companies know that. They market to fear - fear of pills, fear of hospitals, fear of being “too medical.” But the real solution isn’t more herbs. It’s better research. The National Institutes of Health just launched a $12.7 million study to track herbal use in pregnancy. That’s a start. But until we have large, long-term studies, we won’t know what’s truly safe. Until then, the safest choice isn’t the one that sounds the most natural. It’s the one you’ve talked about with your doctor - and the one you can prove is safe.Is ginger safe during pregnancy?
Yes, ginger is considered safe for pregnancy nausea when taken in doses under 1,000 mg per day. Multiple studies support its effectiveness and safety for reducing vomiting and nausea in the first trimester. Stick to ginger tea, capsules, or crystallized ginger - avoid concentrated extracts unless approved by your provider.
Can I drink chamomile tea while pregnant?
Occasional, weak chamomile tea is likely fine for most women. But avoid daily use or strong brews. Some studies link chamomile to potential risks like preterm birth and low birth weight. If you use it for sleep, try alternatives like warm milk or magnesium first.
Is raspberry leaf tea good for preparing for labor?
No. While traditionally used for this purpose, recent evidence shows raspberry leaf can trigger contractions and may increase the chance of cesarean delivery. It’s not proven to shorten labor or make birth easier. The American Academy of Family Physicians classifies it as “likely unsafe” for labor induction. Avoid it unless your provider specifically recommends it with strict dosing.
Are herbal supplements regulated like medicine?
No. In the U.S., the FDA doesn’t test herbal supplements for safety or effectiveness before they’re sold. They’re treated like food, not drugs. That means ingredients, potency, and purity can vary between batches - and sometimes contain harmful contaminants. Always look for third-party testing labels like USP or NSF.
What should I do if I already took a herbal supplement during pregnancy?
Stop taking it immediately and tell your provider. Most supplements won’t cause harm if taken once or briefly, but some - like blue cohosh or pennyroyal - can be dangerous even in small doses. Your provider can help you assess risk based on the herb, dosage, and timing. Don’t panic, but don’t ignore it either.






Casey Mellish
Ginger’s the only herb I’d trust in pregnancy-every other ‘natural’ remedy feels like Russian roulette with a side of marketing hype. I’m Australian, and even here, where we love our echinacea and manuka, midwives are screaming about the lack of regulation. If it’s not in a clinical trial, don’t risk it.
Tyrone Marshall
It’s wild how we treat herbs like they’re harmless because they grow in the ground. But if you poured concentrated rosemary extract into a glass and drank it, you’d be rushed to the ER. Why is it different when it’s in a capsule labeled ‘organic’? We’ve got this weird cultural blind spot where ‘natural’ = safe, even when the science says otherwise. It’s not anti-science to want proof-it’s basic caution.
Emily Haworth
EVERYTHING IS A LIE. 😱 The FDA is in bed with Big Herbal. I found a study that said raspberry leaf tea was linked to a secret government program to lower birth rates. 🤫 I saw it on a forum. Also, my cousin’s neighbor took ginger and her baby was born with three toes. 🍃👶 It’s not coincidence. They don’t want you to know. #NaturalIsNotSafe #BigGinger
Tom Zerkoff
While I appreciate the thoroughness of the original post, I must emphasize the epistemological limitations inherent in extrapolating clinical data from non-pregnant populations to expectant mothers. The absence of robust, longitudinal, double-blind, placebo-controlled trials specific to gestational populations renders nearly all herbal supplementation recommendations speculative at best. The ethical imperative to avoid fetal harm has, paradoxically, created a knowledge vacuum that commercial interests have exploited with alarming efficacy.
Yatendra S
So... if nature made it, why are we scared? 🤔 In India, we’ve used ashwagandha and tulsi for centuries. Is it because Western medicine doesn’t understand it? Or because they can’t patent it? Maybe the real danger isn’t the herbs-it’s the system that profits from pills and ignores tradition. Just saying.
Himmat Singh
It is a fallacy to equate ‘natural’ with ‘safe.’ Indeed, arsenic is natural. Cyanide is natural. The assertion that herbal supplements are inherently benign is not merely inaccurate-it is dangerously misleading. The regulatory framework of the United States, while imperfect, exists precisely to prevent such irrational risk-taking. One cannot logically defend the consumption of unregulated botanical extracts while simultaneously advocating for evidence-based medicine.
kevin moranga
Hey, I get it-pregnancy makes you want to do everything right. But here’s the thing: you’re not alone in this. I’ve seen so many moms stress themselves out over ‘what’s safe’ when the real answer is just: talk to your doc. Ginger tea? Cool. Raspberry leaf? Maybe skip it. But don’t let fear of the unknown make you feel guilty for wanting to feel better. You’re doing great. Seriously. Even if you took something you’re not sure about, it’s not the end of the world. Just tell your provider, breathe, and keep going. You’ve got this.
Alvin Montanez
Let me be clear: if you’re taking anything during pregnancy that isn’t prescribed by a licensed medical professional, you are not being ‘empowered’-you’re being manipulated. These supplement companies are targeting your fears, your guilt, your desire to be a ‘good mom.’ They sell you hope dressed up as wisdom. And when something goes wrong-because it will-you’ll be left holding a bottle with no answers. You don’t need a ‘natural’ fix. You need a doctor. Stop letting influencers decide what’s safe for your child.
Lara Tobin
I took chamomile tea every night for three months. I felt so calm. But now I’m terrified I did something wrong. 😔 I didn’t know about the preterm birth risk. I just wanted to sleep. I told my partner, and he said ‘it’s fine, you’re fine.’ But I don’t feel fine. I just keep thinking… what if? I wish someone had warned me. Not to scare me… just to tell me the truth.
Jamie Clark
You call this ‘evidence’? A 2023 review? That’s not science-that’s a footnote. Real science requires decades of data, not some corporate-funded ‘study’ with 47 participants. And don’t get me started on the FDA-they’re a joke. The only reason ginger is ‘safe’ is because it’s too cheap to patent. If it made money, they’d ban it and sell you a synthetic version for $200 a bottle. Wake up.
Keasha Trawick
Okay, so imagine your uterus is a velvet-lined opera house. Ginger? The understudy who shows up on time, hits the note, and leaves quietly. Raspberry leaf? That’s the diva who storms in at 3am, turns up the bass, and starts belting ‘Nessun Dorma’ while the baby’s trying to nap. The docs? They’re the stage managers screaming ‘NO!’ but the crowd’s too busy chanting ‘TRADITION!’ to listen. And the label? A glittery lie with a tiny ‘may contain traces of contractions.’ 🎭🍼
Webster Bull
ginger = good. everything else = maybe not. talk to your doc. easy. 🙌
Bruno Janssen
I took raspberry leaf. I didn’t know it was risky. Now I’m here. Alone. Scared. I didn’t mean to. I just wanted to feel in control. I don’t even know if I did something wrong. I just… I just wanted to be normal.
Scott Butler
Why are we even having this conversation? In America, we’ve got the best doctors, the best labs, the best science. If you’re taking herbs because you don’t trust your OB-GYN, maybe you need a new doctor-not a new tea. This isn’t Europe. We don’t need to go back to the 1700s to have a healthy baby. Modern medicine works. Stop romanticizing herbal nonsense.