The U.S. pharmaceutical supply chain handles over 5 billion prescription drug transactions every year. For decades, there was no reliable way to know if a pill came from a legitimate manufacturer-or if it was a fake made in a basement lab. That changed with the Drug Supply Chain Security Act (DSCSA), a federal law designed to block counterfeit drugs before they reach your medicine cabinet.
What the DSCSA Actually Does
The DSCSA, signed into law in 2013, didn’t just add another layer of paperwork. It built a digital highway for prescription drugs-one that tracks every bottle, vial, and blister pack from the factory to the pharmacy. By November 27, 2024, every trading partner in the chain-manufacturers, wholesalers, repackagers, and pharmacies-must use electronic systems to verify the authenticity of each drug package. Before DSCSA, drug tracing was a mess. Each state had its own rules. Some required paper logs. Others used outdated barcodes. Counterfeiters exploited those gaps. Now, every package must have a unique serial number, lot number, expiration date, and National Drug Code (NDC)-all printed in both human-readable text and machine-scannable form. This isn’t just about scanning a barcode. It’s about verifying that the product’s digital history matches what’s supposed to be in the supply chain. If a pharmacy receives a box of insulin with a serial number that doesn’t exist in the manufacturer’s database, the system flags it immediately. That’s how fake drugs get caught.How the System Works: The Three Key Pieces
For every drug shipment, three pieces of electronic data must be exchanged between trading partners:- Transaction Information (TI): What’s being shipped-product name, NDC, serial number, quantity, and who sent it.
- Transaction History (TH): A chain of custody showing every stop the product made from manufacturer to dispenser.
- Transaction Statement (TS): A legal certification that the product was handled according to DSCSA rules.
Why This Matters for Patients
Counterfeit drugs aren’t just scams-they’re deadly. Fake versions of blood thinners, antibiotics, and cancer treatments have been found with no active ingredient, wrong dosage, or toxic contaminants. The FDA estimates the DSCSA will reduce counterfeit drug incidents by 95% by 2027. But it’s not just about fakes. The system also stops diverted drugs-medications stolen from warehouses or sold illegally online. Before DSCSA, a thief could steal a pallet of opioids, repackage them, and sell them to a small pharmacy. Now, that serial number gets flagged the moment it’s scanned. McKesson reported a 40% drop in drug diversion after implementing DSCSA-compliant systems. Even recalls are faster and smarter. In the past, if one batch of a drug was contaminated, companies had to recall entire product lines. Now, they can pinpoint the exact lot number and pull only the affected packages. CVS Health cut its suspect product investigations by 75% after automating verification.
Who’s Complying-and Who’s Struggling
Large manufacturers and wholesale distributors are mostly caught up. As of mid-2023, 98% of manufacturers and 95% of wholesalers had full serialization systems in place. The real challenge? Pharmacies. Only 72% of all pharmacies are fully compliant. Independent pharmacies, which serve 1 in 5 Americans, are falling behind. A 2023 survey by the National Community Pharmacists Association found that 68% of independent pharmacists said DSCSA compliance was their biggest technology hurdle. Why? Cost. Upgrading systems to handle electronic verification can cost between $100,000 and $185,000 per pharmacy. Walgreens spent $120 million on DSCSA tech upgrades between 2021 and 2022. For a small, family-run pharmacy, that’s a massive investment. There’s also technical friction. Different software vendors use slightly different versions of EPCIS. Data mismatches-like a serial number that looks right but doesn’t match the manufacturer’s database-are causing delays. Some pharmacies report 2-3 day waits just to verify a shipment.The Tech Behind the System
The DSCSA doesn’t rely on one company’s software. It’s built on open standards. GS1, the global organization that manages barcodes, set the rules for serial numbers: 20-character alphanumeric codes that can’t be duplicated. Each code is unique to one package. Software vendors like TraceLink, SAP, and Oracle dominate the market. TraceLink alone handles over a third of all DSCSA transactions. Their platforms connect manufacturers, distributors, and pharmacies into a single network. When a pharmacy receives a shipment, their system automatically checks every serial number against the manufacturer’s database in seconds. But it’s not just software. It’s people. Companies are hiring DSCSA compliance officers-specialists who understand both pharmaceutical logistics and data standards. Salaries for these roles range from $95,000 to $130,000 a year. The FDA offers free training through its DSCSA Learning Portal. Most compliant companies use these resources. In fact, 87% of surveyed firms said they relied on FDA and industry guides during implementation.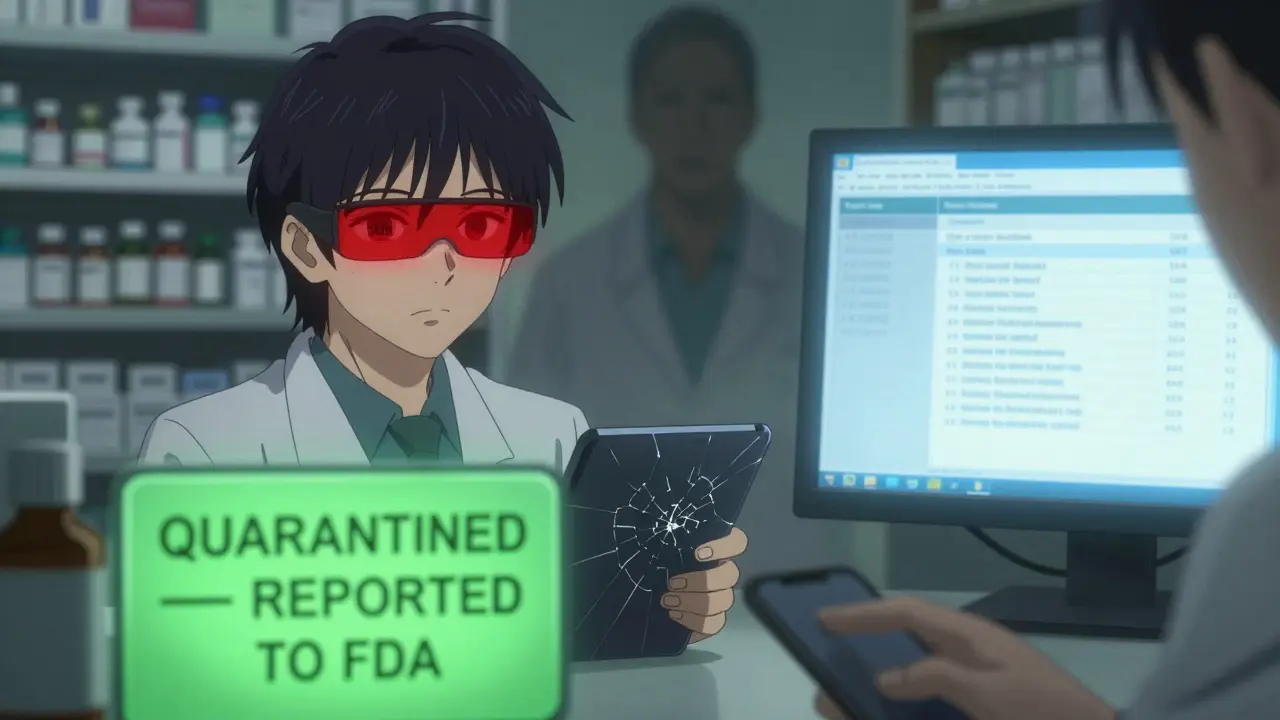
What Happens After November 2024?
The November 27, 2024 deadline isn’t the finish line-it’s the starting line. The FDA will begin stricter enforcement. Companies that still can’t verify products electronically will face warnings, fines, or even suspension of their ability to distribute drugs. The agency is already looking ahead. In March 2023, FDA Commissioner Dr. Robert Califf said the agency is evaluating whether to extend DSCSA rules to certain over-the-counter drugs-especially high-risk ones like insulin pens or erectile dysfunction medications. Long-term, the system could save the U.S. healthcare system over $2 billion a year by reducing waste from bad recalls, cutting down on counterfeit drug lawsuits, and preventing hospitalizations caused by fake medications.What You Can Do
As a patient, you don’t need to understand EPCIS or GS1 standards. But you can stay informed:- If you buy medications online, stick to licensed U.S. pharmacies. Look for the VIPPS seal.
- Check your prescription labels. If the serial number looks smudged or handwritten, ask your pharmacist to verify it.
- Report anything suspicious. If a pill looks different or doesn’t work like it should, tell your pharmacist or report it to the FDA’s MedWatch program.
What is the DSCSA and why was it created?
The Drug Supply Chain Security Act (DSCSA) is a U.S. federal law passed in 2013 to build a secure, electronic system for tracking prescription drugs from manufacturer to pharmacy. It was created to stop counterfeit, stolen, or contaminated drugs from entering the legal supply chain. Before DSCSA, there was no national standard for drug tracing, making it easy for fake medications to slip through.
Does the DSCSA apply to over-the-counter drugs?
Currently, the DSCSA only applies to prescription drugs. But the FDA is evaluating whether to extend the requirements to certain high-risk over-the-counter medications, like insulin pens or erectile dysfunction drugs, especially those that have been targeted by counterfeiters in the past.
How do pharmacies verify a drug’s authenticity under DSCSA?
Pharmacies use scanning systems that read the unique serial number on each drug package. That number is checked against the manufacturer’s database in real time. If the serial number doesn’t match, or if the product’s transaction history is incomplete or missing, the system flags it as suspect. The pharmacy must then quarantine the product and report it to the FDA within 24 hours.
What happens if a pharmacy can’t verify a drug?
If a pharmacy can’t verify a drug’s legitimacy, it must not dispense it. The product is quarantined, and the pharmacy must investigate the issue. If it’s confirmed as counterfeit or illegitimate, the pharmacy must report it to the FDA. Failure to do so can result in regulatory action, including fines or loss of licensing.
Are generic drugs covered by DSCSA?
Yes. DSCSA applies to all prescription drugs sold in the U.S., including generics. Every package-whether brand-name or generic-must have a unique serial number and full electronic transaction data. Counterfeiters often target generics because they’re cheaper and less scrutinized, making DSCSA’s traceability even more critical for these medications.
How has DSCSA affected drug prices?
DSCSA hasn’t directly raised drug prices. But compliance costs-like software upgrades and staff training-have increased operational expenses for pharmacies and distributors. These costs are absorbed into the supply chain, but they’re not passed directly to patients as higher list prices. The long-term savings from fewer counterfeit-related hospitalizations and more efficient recalls are expected to outweigh these costs.
Can patients trust their medications now?
Yes-more than ever. Before DSCSA, there was no reliable way to confirm a drug’s origin. Now, every prescription drug in the U.S. supply chain has a digital fingerprint. While no system is 100% foolproof, the DSCSA has made it exponentially harder for counterfeit drugs to reach patients. The FDA estimates counterfeit incidents will drop by 90% by 2027 thanks to this system.





Michael Burgess
Just saw a pharmacist scan a bottle at my local CVS last week - took 3 seconds. The screen lit up green like a video game confirmation. No more guessing if that $40 insulin is legit. This system? It’s quiet, it’s invisible… and it’s saving lives. 🙌
JUNE OHM
So now the feds are tracking every pill you take? Cool. Next they’ll put GPS chips in your Tylenol. Who’s really behind this? Big Pharma? The FDA? Or some Silicon Valley ghost writing algorithms for ‘supply chain transparency’? 🤔
Kerry Howarth
Compliance isn’t sexy, but it’s necessary. Pharmacies that delay upgrades are putting patients at risk. Time to prioritize safety over savings.
Shruti Badhwar
As someone who works in pharma logistics in India, I’ve seen how counterfeit drugs thrive in fragmented systems. The DSCSA model is revolutionary - but expensive to replicate globally. The real win? The open EPCIS standard. It’s scalable, vendor-neutral, and could become the global baseline. We need this in emerging markets - not just the U.S.
Haley Parizo
They say ‘95% reduction’ - but what about the 5% that still slip through? And who’s auditing the auditors? The same companies that built the software? The FDA doesn’t even have enough staff to inspect 1% of the shipments. This is theater dressed as security. We’re being sold a fantasy.
Brittany Wallace
It’s wild to think that 10 years ago, we were just hoping a pill wasn’t made in a basement. Now we’ve got digital passports for medicine. 🌍💊 I remember my grandma taking her blood pressure meds - she’d stare at the bottle like it might betray her. Now, she just scans it. She doesn’t know how it works… but she trusts it. That’s progress.
Angela Goree
Why are we letting foreign manufacturers dictate our drug supply?! This system should’ve been built with U.S.-only tech, U.S.-only servers, U.S.-only data centers! Now we’re trusting TraceLink - a company that’s got offices in 12 countries - to protect our pills?! This isn’t security - it’s surrender!
Shanahan Crowell
Small pharmacies are getting crushed here. $185k to upgrade? That’s a house payment. The government should be offering grants - not fines. We need to fix this before the deadline hits and folks start running out of meds because their local pharmacy can’t verify a shipment. This isn’t about tech - it’s about equity.
Angela Fisher
Think about it - every time you take a pill, someone somewhere is tracking it. Your name, your doctor, your pharmacy, your insurance - all linked to that serial number. What happens when the database gets hacked? What if the government starts denying your meds based on your ‘risk profile’? What if your insulin gets flagged because you missed a co-pay? This isn’t safety - it’s control. And they’re calling it progress. I’m not buying it. 🚨
Tiffany Channell
Let’s be real: this whole system exists because Big Pharma got caught shipping fake generics to the VA. The DSCSA isn’t about patient safety - it’s about liability protection. They got sued, they panicked, and now they’ve built a $20 billion paper fortress to hide behind. Meanwhile, insulin still costs $300. Funny how that works.
Ian Detrick
The real genius here isn’t the tech - it’s the collaboration. Manufacturers, distributors, pharmacies - all agreeing to share data in real time. That’s never happened before in healthcare. It’s messy. It’s slow. But it’s working. We’re building trust in a system that used to be built on lies.
Philip Leth
My uncle runs a small pharmacy in rural Ohio. He told me last month he’s still using a 2018 scanner and printing out paper logs. He’s got 3 employees. He can’t afford the upgrade. He’s scared. He’s not lazy - he’s stuck. If we don’t help him, someone’s gonna get hurt. And it won’t be because of fakes - it’ll be because the system broke for people who can’t afford to play.
Joy F
Let’s not romanticize this. The DSCSA is a bureaucratic Rube Goldberg machine built on open standards that no one fully understands. EPCIS? GS1? NDC? Who even wrote these acronyms - a committee of accountants who hate humans? The system works… technically. But it’s brittle. One mismatched character in a serial number and the whole thing freezes. Pharmacies are stuck in limbo for days. Patients are confused. And the FDA? They’re just watching. This isn’t innovation - it’s institutional inertia with a shiny UI.