Imagine looking at a loved one’s face and not being able to make out their eyes. Or trying to read the clock on the wall, but the numbers are blurred, broken, or missing in the center. This isn’t just poor eyesight-it’s age-related macular degeneration, or AMD. It’s the number one cause of vision loss in people over 55 in the UK and the US, and it doesn’t take your sight completely-it steals the part you need most to live fully.
What Exactly Is AMD?
AMD attacks the macula, a tiny spot in the center of your retina. This is where your sharpest vision lives. It’s what lets you read, drive, recognize faces, and see fine details. When the macula breaks down, you lose that central vision. But your side vision? That stays sharp. You can still walk around without bumping into things, but you can’t see the face of the person you’re talking to. There are two types: dry and wet. Dry AMD is the most common-about 9 out of 10 cases. It starts with tiny yellow deposits called drusen building up under the retina. Over time, the cells in the macula thin out and die. This is called geographic atrophy. It’s slow. It creeps up. You might not notice it for years. Wet AMD is the scary one. It makes up only 10-15% of cases, but it causes 90% of severe vision loss. Here, abnormal blood vessels grow under the retina. They leak fluid and blood like broken pipes. This messes up the delicate layers of the macula, and vision can crash in weeks or months. Dry AMD can turn into wet AMD at any time. That’s why monitoring your vision matters.Who’s at Risk?
Age is the biggest risk. Less than 1% of people in their 40s have AMD. By age 75, that jumps to 35%. But age isn’t the whole story. Smoking is the number one modifiable risk. If you smoke, you’re nearly four times more likely to develop AMD than someone who never did. Quitting helps-even after years of smoking. Genetics play a huge role. If a parent or sibling has AMD, your risk goes up 3 to 6 times. White people are more likely to get it than Black or Hispanic people. High blood pressure, high cholesterol, and being overweight also raise your odds. It’s not just about what you do now-it’s what’s been building up for years. Oxidative stress, inflammation, and damage to the retinal pigment layer slowly wear down the macula. Think of it like rust on a car. You don’t see it until it’s too late.How Anti-VEGF Therapy Stops Vision Loss
This is where anti-VEGF treatment comes in. VEGF stands for vascular endothelial growth factor. It’s a protein your body makes to grow new blood vessels. That’s useful when you’re healing a wound. But in wet AMD, your body makes too much of it-too late, in the wrong place. The result? Leaky, fragile blood vessels under your retina. Anti-VEGF drugs block that protein. They stop the bad vessels from forming and seal off the ones already there. The treatment? A tiny injection into the eye. It sounds scary, but it’s quick. Most people feel pressure, not pain. Local numbing drops make it tolerable. This isn’t a cure. But it’s the most effective tool we have. Without treatment, wet AMD can turn 20/200 vision into legal blindness in under a year. With regular anti-VEGF shots, most people stop losing vision. About two in three see improvement. One patient on Reddit shared: “After 12 injections over nine months, my vision went from 20/200 to 20/40. Worth every uncomfortable moment.”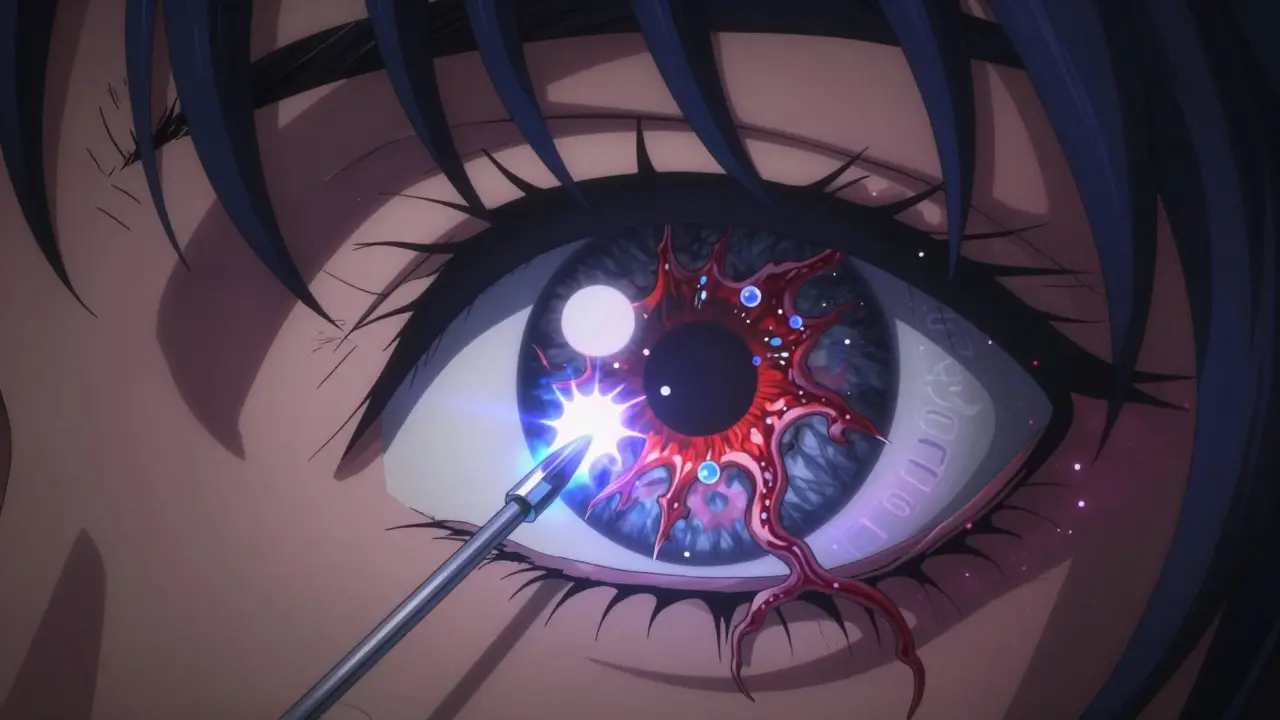
What Does Treatment Look Like?
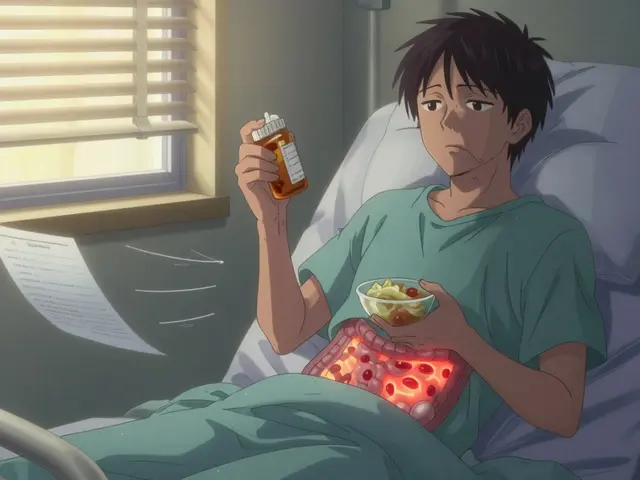
It’s not a one-and-done fix. You start with monthly injections for three months. Then, your doctor checks your eyes with an OCT scan-a non-invasive image that shows swelling and fluid in the retina. If fluid’s still there, you get another shot. If it’s gone, you wait. Some people need shots every 4 weeks. Others can stretch it to 8 or even 12 weeks as their condition stabilizes. Newer treatments are making this easier. In 2021, the FDA approved Susvimo, a tiny implant that slowly releases ranibizumab for up to six months. That cuts down on visits. In 2022, Vabysmo came out-a drug that blocks two targets at once (VEGF and another protein called angiopoietin-2), which means fewer injections for some patients. Still, the burden is real. Eighty-two percent of patients say frequent clinic visits are their biggest challenge. Miss one injection, and you risk losing vision. Studies show people who skip more than a quarter of their shots lose 30% more vision than those who stick to the plan.What Else Can You Do?
Treatment isn’t just about shots. Lifestyle matters. The AREDS2 formula-a specific mix of vitamins and minerals-is proven to slow progression in dry AMD. It includes vitamin C, vitamin E, zinc, copper, lutein, and zeaxanthin. It doesn’t help everyone, but for those with intermediate AMD, it cuts the risk of turning wet by 25%. Eat more leafy greens. Fish rich in omega-3s. Avoid processed foods and sugar. Control your blood pressure and cholesterol. Quit smoking. These aren’t just “good ideas”-they’re backed by decades of research. And don’t ignore the Amsler grid. It’s a simple checkerboard pattern you can use at home. If the lines start to look wavy, broken, or missing in the center, call your eye doctor right away. Four in ten people catch wet AMD early using this tool before their next appointment.
What’s Next for AMD Treatment?
Science is moving fast. Gene therapy trials are underway, targeting the genes linked to half to 70% of AMD cases. Early results show promise in slowing down the immune system’s attack on the retina. Longer-lasting drugs are being tested. Some are designed to work for 6 months or more. Others are being delivered through eye drops instead of injections-something that would change everything for patients. The goal isn’t just to stop vision loss. It’s to restore it. Researchers are testing retinal implants and stem cell therapies. They’re not ready yet, but the direction is clear: we’re moving from managing AMD to reversing it.Living With AMD
AMD doesn’t mean the end of a full life. It means adapting. Many people use magnifiers, screen readers, and voice assistants. Bright lighting helps. High-contrast settings on phones and tablets make reading easier. Support groups matter. Talking to others who get it reduces anxiety. The Fighting Blindness Foundation found that 78% of AMD patients struggle to read, 65% can’t recognize faces, and over half can’t drive. But with treatment and support, most keep living independently. The key is catching it early. Annual eye exams after 65 aren’t optional-they’re essential. If you have risk factors, go sooner. If you notice changes in your central vision, don’t wait. Call your eye doctor. Now.What If I’m Already Diagnosed?
If you’ve been told you have dry AMD, start the AREDS2 supplements. Quit smoking. Monitor your vision daily with the Amsler grid. Get checked every 6 to 12 months. If you’ve been diagnosed with wet AMD, start anti-VEGF treatment right away. Don’t delay. Every week counts. Stick to your injection schedule. Ask your doctor about longer-acting options like Susvimo or Vabysmo if you’re tired of monthly visits. You’re not alone. Over 10 million Americans and millions more worldwide live with AMD. And thanks to anti-VEGF therapy, most of them are still reading, still driving, still seeing their grandchildren’s faces.Can AMD be cured?
No, AMD cannot be cured yet. But wet AMD can be managed very effectively with anti-VEGF injections, which often stop vision loss and sometimes even improve it. Dry AMD can be slowed with supplements and lifestyle changes. The goal is to preserve vision for as long as possible.
Are anti-VEGF injections painful?
Most people feel only pressure or a slight sting. The eye is numbed with drops before the injection, and the procedure takes less than a minute. Many patients say the fear is worse than the actual shot. Anxiety drops after the first few visits.
How often do I need anti-VEGF injections?
Initially, you’ll get one injection every month for three months. After that, your doctor will use OCT scans to check for fluid in your eye. If there’s no fluid, you may go 8 to 12 weeks between shots. Some patients need injections every 4 weeks long-term. Newer treatments like Susvimo or Vabysmo can extend the time between visits.
Can I use over-the-counter eye drops for AMD?
No. Over-the-counter eye drops won’t help AMD. They might relieve dryness or redness, but they don’t stop the underlying damage. Only prescription treatments like anti-VEGF injections or the AREDS2 supplement have been proven to affect AMD progression.
Does smoking really make AMD worse?
Yes. Smokers are nearly four times more likely to develop AMD than non-smokers. Smoking speeds up damage to the retina and reduces the effectiveness of treatments. Quitting at any stage reduces your risk and improves treatment outcomes.
Is AMD hereditary?
Yes. If a close family member has AMD, your risk is 3 to 6 times higher. Genetic testing isn’t routine yet, but knowing your family history helps your doctor monitor you more closely.
Can I still drive with AMD?
It depends on how much central vision you’ve lost and your country’s legal requirements. In the UK, you must be able to read a number plate from 20 meters. Many people with AMD can still drive with low-vision aids, but others need to stop. Always check with your eye doctor and the DVLA.
What’s the difference between dry and wet AMD?
Dry AMD is slower, caused by drusen buildup and thinning of the macula. Wet AMD is sudden and dangerous, caused by leaking blood vessels. Dry AMD can turn into wet AMD at any time. Wet AMD causes rapid vision loss without treatment. Anti-VEGF injections only work for wet AMD.




Peter Sharplin
Had a friend go through this last year. Started with the Amsler grid, caught it early. Now she’s on Vabysmo and her vision’s stable. Monthly shots were hell at first, but she says the fear was worse than the actual thing. Now she’s back reading to her grandkids. It’s not a cure, but it’s a lifeline.
Biggest thing? Don’t wait. If your central vision’s off, even a little, get it checked. AMD doesn’t ask for permission.
John Wippler
AMD’s like watching your favorite book get slowly erased page by page - the words are still there, but the heart of the story? Gone. Anti-VEGF doesn’t rewrite the chapters, but it stops the bleach from spreading.
I’ve seen people go from ‘I can’t see my dog’s face’ to ‘I can see the whiskers twitching.’ That’s not medicine. That’s magic with a syringe.
And yeah, smoking? It’s not just ‘bad for you.’ It’s like pouring acid on your retina and calling it a habit. Quitting isn’t a suggestion - it’s the first injection you never get.
rasna saha
My mom has dry AMD. She takes the AREDS2 pills every day like clockwork. Says it’s her ‘eye vitamins.’ She doesn’t know the science, but she knows it keeps her reading her Bible. That’s enough for her.
Also, she uses a magnifying lamp now. Looks like a scientist from the 1950s, but she’s reading recipes again. Small wins, right?
Skye Kooyman
Just got diagnosed with early dry AMD. Started the AREDS2. No injections yet. Fingers crossed.
Uche Okoro
The pathophysiology of neovascular AMD is fundamentally driven by hypoxia-induced upregulation of VEGF-A isoforms via HIF-1α signaling cascades in retinal pigment epithelial cells. Anti-VEGF agents like ranibizumab and aflibercept competitively inhibit VEGF receptor binding, thereby suppressing choroidal neovascularization and vascular permeability.
However, the pharmacokinetic half-life of intravitreal injections remains suboptimal, necessitating frequent dosing regimens that compromise adherence. Emerging sustained-release platforms, such as the Susvimo pump, demonstrate a 60% reduction in injection frequency with non-inferior visual outcomes in Phase III trials.
Further, the dual inhibition of VEGF and Ang-2 by Vabysmo (faricimab) modulates pericyte recruitment, enhancing vascular stability beyond VEGF blockade alone. This represents a paradigm shift from reactive to proactive vascular modulation.
Ashley Porter
Just read the part about OCT scans. That’s the real MVP here. It’s not the injection - it’s the imaging. Without those cross-sections of the retina, you’re flying blind. Literally.
Doctors who skip OCT and just go on ‘feel’ are doing their patients a disservice. The fluid doesn’t lie. The scans do.
shivam utkresth
Back home in Kerala, my uncle had AMD. He didn’t have access to injections. So he ate spinach every day, drank coconut water, and did eye exercises his grandfather taught him. His vision didn’t get better - but it didn’t get worse either.
Maybe the science is in the lab, but the wisdom? It’s in the kitchen. Don’t dismiss the old ways just because they don’t come in a vial.
Also, the Amsler grid? My aunt printed 20 of them. Taped one to every mirror. Genius.
Kipper Pickens
Anti-VEGF is effective, yes. But the real issue is access. In rural America, getting to a retina specialist every 4-8 weeks is a 3-hour drive, a day off work, and a $200 co-pay. Most patients drop out. That’s not medical failure - it’s systemic failure.
We’re treating the disease like it exists in a vacuum. It doesn’t. It lives in a carpool lane, a bus schedule, a paycheck that’s already stretched thin.
Long-acting drugs? Great. But if you can’t get them to the clinic, they’re just expensive paperweights.
Aurelie L.
I lost my vision. Then I got the shots. Now I see my cat again. That’s all that matters.
Joanna Domżalska
So let me get this straight - you’re telling me we inject poison into people’s eyeballs to stop their body from making a protein that helps healing… but we don’t know why it works long-term?
Also, why are we still using 1990s-era injection tech? Why not just laser the bad vessels? Why not gene editing? This feels like patching a leaky boat with duct tape while the ocean rises.
And don’t even get me started on ‘lifestyle changes.’ You think eating kale fixes decades of oxidative damage? Please. This is Big Pharma’s cash cow. The ‘cure’ is just a subscription.