Every year, over 1.5 million people in the U.S. suffer harm from medication errors - many of them preventable. These aren’t just rare mistakes. They happen because someone missed a decimal point, confused one drug name for another, or didn’t check the strength before giving a pill. The good news? You don’t need to be a doctor to spot these errors. With a few simple checks, you can protect yourself or someone you care about from serious harm.
Start with the Drug Name
The first thing to verify is the medication name. Sounds obvious, right? But look-alike and sound-alike names cause more errors than you’d think. Think of prednisone and prednisolone. Or hydroxyzine and hydralazine. One letter off, and you’re giving a completely different drug.Always compare the name on the prescription to the label on the bottle. If you’re reading an electronic order, make sure the full name appears - no abbreviations. The FDA and ISMP have banned dangerous abbreviations like “U” for units (use “unit”) and “mcg” instead of “μg.” Even “MS” can be deadly - it could mean morphine sulfate or magnesium sulfate. Never assume. If it’s not spelled out clearly, ask.
Many hospitals and pharmacies now use “Tall Man” lettering to reduce confusion. You’ll see PREDNISONE and PREDNISOLONE with the different letters capitalized. This isn’t just formatting - it’s a safety tool. If you’re handed a medication without this, double-check.
Verify the Strength - Every Time
Strength is where most mistakes happen. A 2018 FDA report found that 34% of medication errors involved wrong strength. That’s one in three. And the biggest culprit? Missing units or bad formatting.Look for this: the number, a space, then the unit. “10mg” is dangerous. “10 mg” is safe. That space prevents misreading - like mistaking 10mg for 100mg. The same goes for liquids: “500mcg/mL” should be “500 mcg/mL.” No spaces? That’s a red flag.
For injectables, avoid ratio formats like “1:10,000.” That’s outdated and confusing. The correct way is “epinephrine 0.1 mg/mL.” If you see a ratio, ask for clarification. Between 2010 and 2015, over 200 errors were traced back to people misreading epinephrine ratios.
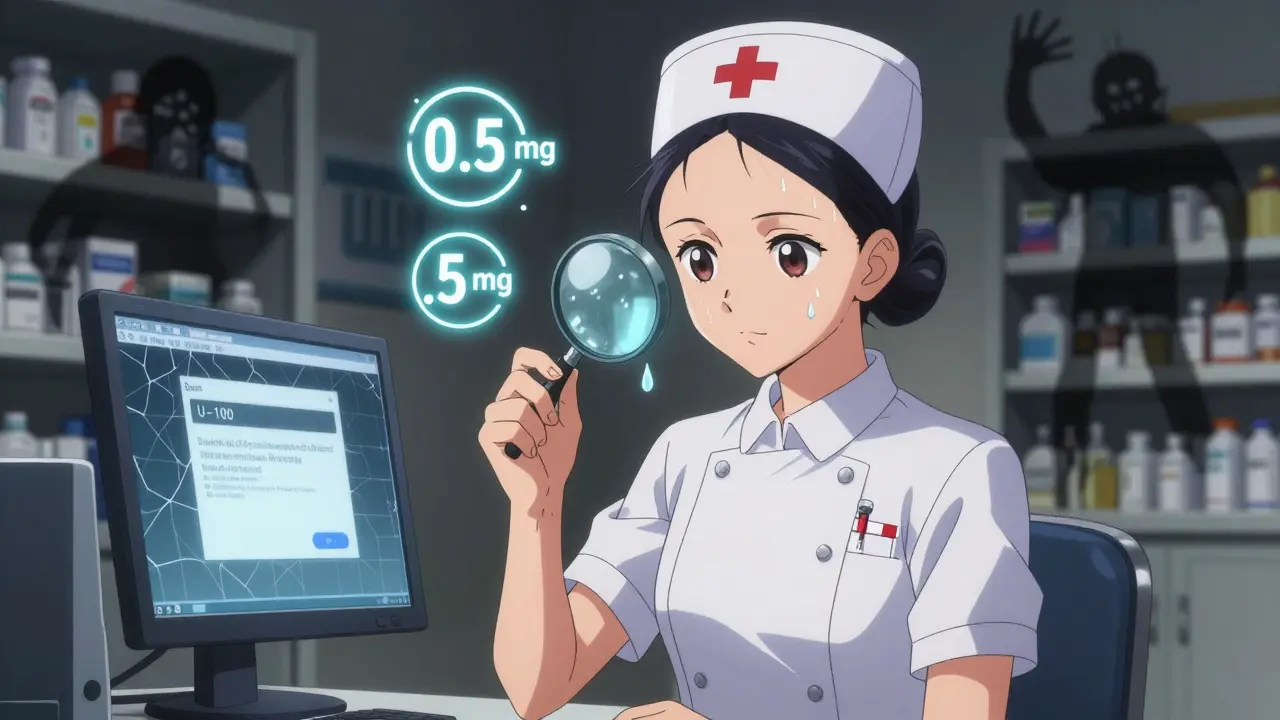
Insulin is another high-risk area. There are 10 different strengths. If you’re given “U-100” insulin, make sure it’s not U-500. A nurse in Texas once nearly gave a patient 100 times too much insulin because the label wasn’t clear. She caught it because she checked the vial against the order. Always do the same.
Dosage Form Matters More Than You Think
The form of the medication - tablet, capsule, liquid, patch, injection - tells you how it’s meant to be used. Giving a tablet meant to be swallowed when it’s actually a sublingual tablet can lead to serious side effects. Or worse - giving an oral liquid as an injection.One Reddit user shared how a relative was given an oral suspension labeled “for oral use only” - but the nurse assumed it was for IV because the bottle looked like an injectable. The patient suffered severe tissue damage. That error happened because the dosage form wasn’t clearly stated on the order.
Always check: Is it a tablet? Capsule? Liquid? Patch? Extended-release? If the order says “amoxicillin 500 mg” but doesn’t say “capsule” or “suspension,” ask. Some forms are designed to release slowly. Crushing an extended-release tablet can cause a dangerous overdose.
Also, watch for “as needed” (PRN) orders. If the form doesn’t match the condition - like a rectal suppository ordered for nausea when the patient can’t swallow - that’s a mismatch. Don’t assume. Confirm.
The Three-Point Verification Rule
Experts agree: verification must happen at three key moments.- When you receive the order - whether it’s from a doctor, nurse, or pharmacy. Check for completeness: name, strength, unit, form, route, frequency. If anything’s missing, don’t proceed.
- When you prepare the medication - before you open the bottle or draw up the syringe. Match the label on the container to the written order. Use the “five rights”: right patient, right drug, right dose, right route, right time.
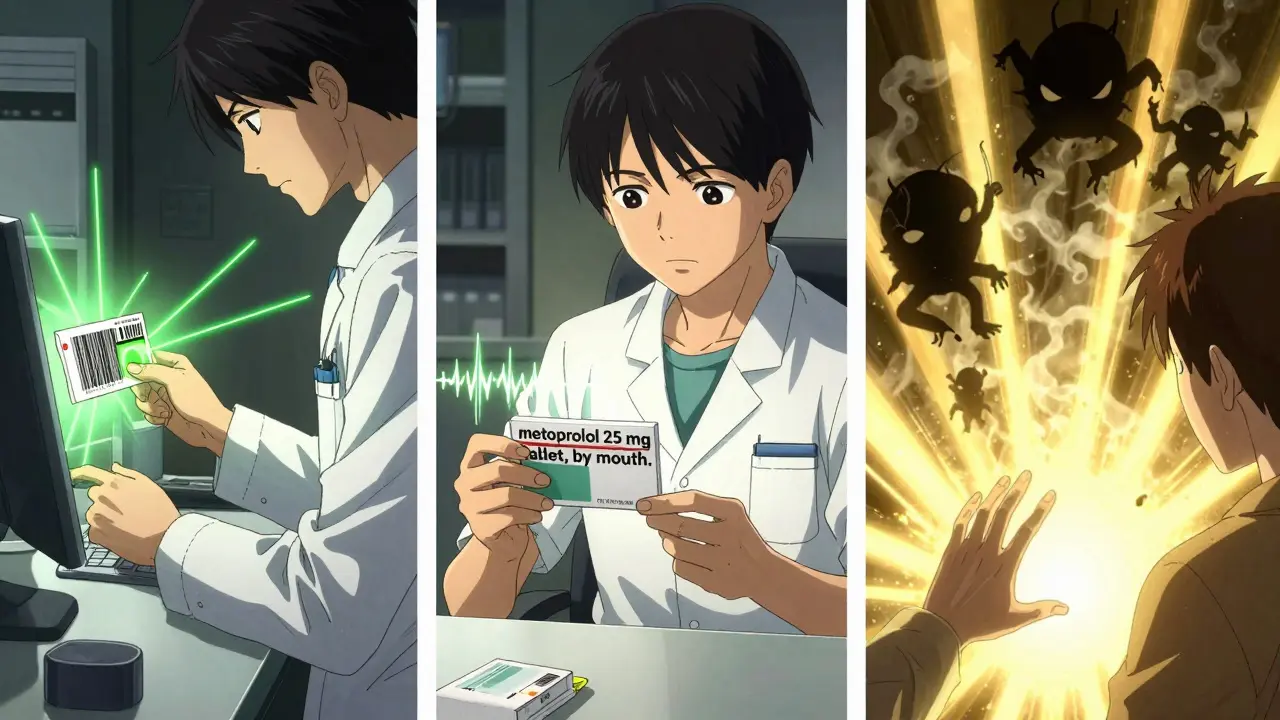
- Right before administration - when you’re standing at the bedside or handing the pill to someone. Say it out loud: “This is metoprolol 25 mg tablet, by mouth, once daily.”
This is called the “read-back” method. A 2023 study in the American Nurses Association forums found that 89% of people who prevented errors used this technique. It’s simple. It’s free. And it works.
Watch for Red Flags in the System
Technology helps - but it can also trick you. Electronic health records (EHRs) flag potential errors, but if you’re used to clicking “approve” without reading, you’re in danger. This is called “automation bias.” A 2020 study found that 18% of errors happened because clinicians ignored alerts because the system said it was fine.Here’s what to do:
- If an alert pops up, don’t dismiss it just because it’s “familiar.”
- If the system auto-fills a drug name, double-check it. It might have picked the wrong one.
- Barcodes on pills? Scan them. A 2020 study showed barcode scanning cut dispensing errors by 83%.
- Is the dosage calculator showing “0.5 mg” and the label says “.5 mg”? That’s the same - but the leading zero matters. Always write “0.5,” never “.5.”
High-alert medications - like insulin, heparin, opioids, and IV potassium - need extra care. Many hospitals now require two people to verify these before giving them. If you’re in a setting without that policy, ask for it. Your life might depend on it.
What to Do If Something Feels Off
You don’t need to be an expert to trust your gut. If the name looks weird, the dose seems too high, or the form doesn’t make sense - stop. Ask again. And again.One nurse in Bristol told me about a time she was given “Heparin 5,000 units/mL” for a patient who needed “50 units/mL.” The label on the vial said 5,000. The order said 50. She didn’t trust the computer. She called the pharmacy. They admitted it was a typo. That one check saved the patient from a fatal bleed.
Never feel embarrassed to ask. Pharmacists, nurses, and doctors expect it. In fact, they’re trained to welcome questions. The most dangerous thing isn’t asking - it’s staying silent.
What You Can Do Right Now
You don’t have to wait for a hospital visit to protect yourself. Here’s your action list:- When you pick up a prescription, read the label aloud. Compare it to the doctor’s note.
- Keep a list of all your meds - names, strengths, forms - in your phone or wallet.
- Ask your pharmacist: “Is this the same as last time? Has anything changed?”
- Use the “read-back” method with caregivers: “So this is lisinopril 10 mg tablet, once a day, by mouth?”
- If you’re giving meds to someone else - a parent, a child, a partner - write it down. Don’t rely on memory.
Medication safety isn’t about memorizing complex rules. It’s about slowing down, asking questions, and trusting your instincts. The system isn’t perfect. But you can be the last line of defense.
What should I do if I find a mistake on my medication label?
Stop. Don’t take the medication. Call your pharmacy or prescriber immediately. Show them the label and the prescription. Most pharmacies will replace it at no cost. If you’re in a hospital, alert the nurse or pharmacist on duty. Never ignore a mismatch - even if it seems small.
Can I trust the computer system to catch all errors?
No. Computer systems catch about 70-80% of potential errors, but not all. They can miss look-alike names, wrong strengths if units are missing, or dosage form mismatches. Automation bias - where people ignore alerts because the system approved it - causes real harm. Always verify manually, even if the screen says it’s fine.
Why is the space between the number and unit so important?
Without a space, “10mg” can be misread as “100 mg” if the “0” is smudged or the “1” looks like a “10.” The ISMP found that adding a space reduces unit misinterpretation errors by 12%. That’s thousands of preventable mistakes every year. Always write “10 mg,” not “10mg.”
Are there any medications that are especially dangerous to get wrong?
Yes. These are called high-alert medications. They include insulin, heparin, morphine and other opioids, IV potassium, and concentrated electrolytes. A mistake with these can cause death in minutes. Always use two-person verification for these, and never assume the dose is correct - even if it’s been given before.
What if my doctor uses abbreviations like “QD” or “BID”?
Ask them to write it out. “QD” (once daily) can be mistaken for “QID” (four times daily). “BID” (twice daily) can be misread as “TID” (three times). The Joint Commission banned these abbreviations in 2004. If your doctor still uses them, request they use “daily,” “twice daily,” etc. Clarity saves lives.




Melissa Melville
So basically if you can read, you’re now a pharmacist? Cool. I’ll just start auditing my grandma’s meds now. 🙃
vivian papadatu
This is the kind of post that should be mandatory reading for every family caregiver. I’ve seen too many elderly relatives nearly overdose because someone skimmed the label. That space between ‘10’ and ‘mg’? It’s not pedantry - it’s a life raft. I print this out and keep it taped to my medicine cabinet.
Deep Rank
ok but like… why do we even have meds that sound the same? like prednisone and prednisolone?? who thought that was a good idea?? it’s like naming two different types of cars ‘Tesla Model S’ and ‘Tesla Model Z’ and then saying ‘oh but they’re different!’ no they’re not, they’re both just death traps with wheels. also i typed this on my phone so sorry for typos but i’m mad and my thumbs are tired. also i work in a pharmacy and this happens every. single. day. and no one listens. and then the patient dies and everyone says ‘oh what a tragedy’ like it was fate. no. it was laziness. and bad design. and corporate greed. and we’re all complicit.
Naomi Walsh
It’s amusing how this article treats medication safety like a novel insight. The Tall Man lettering standard was formalized in 2002 by ISMP. The five rights have been taught since the 1950s. The fact that this is even a ‘discussion’ in 2025 reveals a systemic failure of medical education - not a lack of public awareness. If your pharmacist can’t spell out ‘microgram’ without abbreviating, they shouldn’t be licensed. Period.
Lu Gao
Wait - so you’re saying I should actually READ the label? 😱 I thought the barcode was supposed to do that for me. Also, I just took my insulin and it said ‘U-100’ - but the vial looked like it had a ‘5’ on it? Should I be worried? 🤔
Angel Fitzpatrick
They’re watching. The EHR system doesn’t just flag errors - it logs your hesitation. That ‘pause’ before you press ‘approve’? That’s data. They’re building a behavioral profile. You think this is about safety? Nah. It’s about compliance metrics. They don’t care if you live - they care if you clicked ‘confirm’ fast enough. And if you ask too many questions? They’ll label you ‘high-risk patient.’ Next thing you know, your prescriptions get auto-rejected. Welcome to the algorithmic pharmacy.
Jamie Allan Brown
I’ve worked in hospice for 18 years. The most powerful tool I’ve ever seen isn’t a barcode scanner or a computer alert - it’s a caregiver sitting down with a patient and saying, ‘Let’s read this together.’ No rush. No assumptions. Just two people, one pill, one question: ‘Does this feel right?’ That’s the real safety net. And it costs nothing.
Nicki Aries
Can we PLEASE stop using ‘QD’ and ‘BID’?!! I’ve seen nurses write ‘QD’ and then cross it out and write ‘daily’… and then someone else rewrites it as ‘QID’ because they thought the ‘D’ was a ‘4’… and then the patient got FOUR doses instead of ONE… and I had to sit with the family while they cried… and I still have nightmares. Please. Just. Write. It. Out.
Ed Di Cristofaro
Yeah right. Like I’m gonna stop and double-check every pill when I’m rushing to work. My boss don’t care if I’m dead, he just wants me to show up. So I’ll just take what they give me and hope for the best. That’s life.
Bob Cohen
Honestly? I think this post is great - but you’re missing the real problem: pharmacies are understaffed, overworked, and paid by volume, not accuracy. If you want fewer errors, pay pharmacists more. And hire more of them. No amount of ‘read-back’ will fix a system that treats human lives like inventory.
Lilliana Lowe
It’s frustrating to see this framed as a ‘public safety’ issue when the real failure lies in the absence of standardized nomenclature across pharmaceutical manufacturers. The FDA’s guidelines are advisory, not enforceable. Until ‘prednisolone’ and ‘prednisone’ are legally required to differ by more than one character, we’re just rearranging deck chairs on the Titanic. Also, the term ‘Tall Man’ is misleading - it should be called ‘Differential Capitalization Protocol.’
Ishmael brown
Wait… so if I scan the barcode and the system says ‘correct,’ but I think it looks weird… should I still take it? 🤨