When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. That’s not luck. It’s because of CGMP - Current Good Manufacturing Practices - enforced by the FDA. These aren’t suggestions. They’re legally binding rules that every generic drug maker in the U.S. must follow. If they don’t, the drug gets pulled. The factory shuts down. People get hurt.
What Exactly Is CGMP for Generics?
CGMP stands for Current Good Manufacturing Practices. It’s the set of rules the FDA uses to make sure every batch of a generic drug is safe, pure, and effective. These rules are written into federal law under 21 CFR Parts 210 and 211. They cover everything: who works in the facility, how the building is cleaned, how equipment is calibrated, how ingredients are tested, and how records are kept.The FDA doesn’t treat generics differently from brand-name drugs. A generic tablet must be made under the same standards as the original. That’s not marketing. That’s the law. As Pfizer put it in their 2023 FAQ: generics must be manufactured under the same strict standards as brand products. There’s no loophole. No shortcut.
The "current" in CGMP matters. It means you can’t use 1980s methods just because they worked back then. You have to update your systems. If your facility still uses paper logs for batch records, you’re already out of compliance. Electronic records with audit trails are now standard. The FDA expects you to keep up.
Key Requirements: What the FDA Actually Checks
The FDA doesn’t guess. They inspect. And they check every part of the process. Here’s what they look for:- Personnel: Everyone who touches the product needs training. Not just a one-time class. Annual training. Documented. Signed off. If a technician can’t prove they’ve been trained on cleaning procedures, that’s a violation.
- Facilities: Air quality, humidity, temperature - all controlled. Dust? Not allowed. Cross-contamination? A red flag. Rooms must be designed to prevent mix-ups. Separate areas for different drugs. Even the ventilation system has specs.
- Equipment: Every machine must be cleaned, calibrated, and maintained. Logs must show when it was last checked. If a tablet press hasn’t been calibrated in six months, that’s a problem. Swab tests for cleaning validation? Required. Acceptance limit? No more than 100 CFU per swab for microbial contamination.
- Components: Every batch of active ingredient gets tested. Not just once. Every time. If you’re using glycerin or propylene glycol, you must test for diethylene glycol - a toxic contaminant. The FDA issued an immediate guidance on this in May 2023 after deaths linked to contaminated medicine in Pakistan.
- Production: You can’t just wing it. Every step - mixing, granulating, compressing - must be validated. That means proving your process consistently produces the same result. Most companies use three consecutive batches to prove it. The FDA doesn’t require a minimum number, but industry practice is clear: three is the baseline.
- Lab controls: Stability testing. Potency checks. Dissolution rates. All must be documented. And kept for at least one year after the drug expires. If you can’t pull a batch record from five years ago, you’re not compliant.
- Records: Everything. Paper or electronic. But if it’s electronic, it must follow 21 CFR Part 11. That means secure login, audit trails, data integrity. No editing past entries. No deleting logs. The FDA has cracked down hard on data manipulation. In 2022, 63% of all warning letters for data integrity issues came from foreign facilities.
Why CGMP Matters More Than You Think
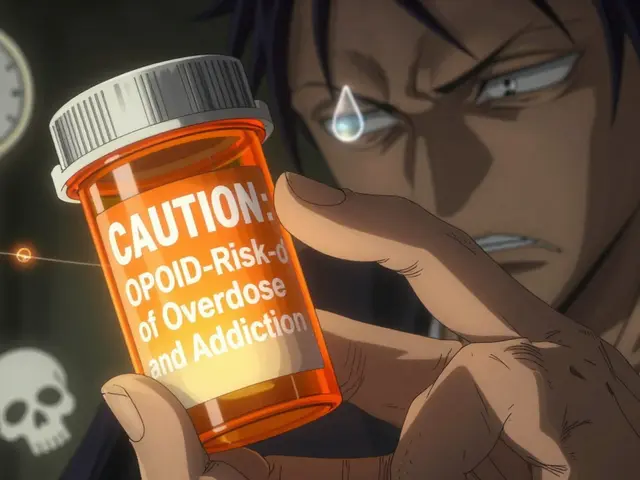
In 2022, 90% of all prescriptions filled in the U.S. were for generic drugs. That’s $105 billion in sales. But behind every pill is a factory. And if that factory cuts corners, people die.Take the 2022 metformin recalls. Over a dozen generic versions were pulled because of NDMA, a probable carcinogen. The FDA blamed inadequate process controls and failed cleaning validation. Not a single pill was tested for that contaminant before it reached patients.
Or the 2020-2022 pandemic. Nearly 40% of U.S. drug shortages were linked to CGMP failures - not lack of raw materials, but factories that couldn’t pass inspection. One plant in India got shut down for 18 months because their water system didn’t meet purity standards. That one facility supplied 15% of the country’s generic antibiotics.
CGMP isn’t about bureaucracy. It’s about preventing preventable harm. A mislabeled bottle. A contaminated batch. A machine running out of calibration. These aren’t theoretical risks. They’ve happened. And they’ll happen again if standards slip.
How Big vs. Small Manufacturers Handle CGMP
Not all generic makers are the same. Big companies like Teva, Mylan, and Sandoz have teams of regulatory experts, dedicated QA departments, and millions in compliance budgets. Small companies? They’re struggling.A 2022 survey of 317 generic manufacturers found that 68% said documentation was their biggest headache. One small company on Reddit spent $1.2 million and 14 months just to switch from paper to electronic batch records. That’s not a cost of doing business - that’s a survival cost.
The numbers show the gap:
- Large manufacturers (> $1B revenue): 97% CGMP compliance rate
- Small manufacturers (< $100M revenue): 82% compliance rate
Why? It’s not that small companies are lazy. It’s that compliance is expensive. The Avalere Health study found CGMP adds 18% to manufacturing costs. For a small firm, that’s the difference between profit and loss.
But here’s the twist: the FDA inspects domestic facilities 1.3 times a year on average. Foreign facilities? Less than half that. A 2021 Harvard study found foreign plants got 43% fewer warning letters per inspection than U.S. ones. That’s not fair. And it’s risky.
What’s Changing in 2024 and Beyond
The FDA isn’t standing still. Their 2023-2027 plan says they’re shifting to risk-based inspections. More resources going to foreign plants. More focus on data integrity. More scrutiny on supply chains.Here’s what’s coming:
- Continuous manufacturing: Traditional batch production is being replaced by continuous flow systems. Think of it like a factory assembly line instead of making one batch at a time. Teva already did it for a heart drug - cut batch failures from 4.2% to 0.7%. The FDA is drafting new guidance for this in Q2 2024.
- AI and predictive quality: By 2028, 65% of manufacturers are expected to use AI to predict quality issues before they happen. Real-time monitoring. Automated alerts. This isn’t sci-fi. It’s the next step in CGMP.
- Supply chain security: The Drug Supply Chain Security Act is forcing manufacturers to track every ingredient from source to shelf. You can’t just buy API from a random supplier anymore. You need proof of testing, certification, and audit history.
- Part 11 enforcement: 73% of industry leaders expect tighter rules on electronic records. Audit trails must be tamper-proof. No more "I didn’t know how to use the system" excuses.

What Happens If You Don’t Comply?
The FDA doesn’t warn you twice. They don’t give you a pass because you’re "trying your best."Non-compliance means:
- Warning letters - public record
- Import alerts - your drugs get blocked at the border
- Consent decrees - court orders forcing you to fix everything under court supervision
- Civil penalties - up to $1 million per violation
- Product recalls - cost you millions and destroy your reputation
Janet Woodcock, former head of FDA’s drug center, said it plainly: non-compliance can lead to a ban on selling your drug. That’s it. No second chances. No appeals. Just shut down.
How to Get Started Right
If you’re starting a generic drug facility, here’s how to avoid disaster:- Build your Quality Management System (QMS) first - before you buy a single machine. Document everything.
- Train your staff. Not once. Every year. Keep records.
- Qualify your facility: Installation Qualification (IQ), Operational Qualification (OQ), Performance Qualification (PQ). Don’t skip any.
- Validate your processes. Use three consecutive batches. Document every parameter.
- Go electronic. Paper is a liability. Use an eQMS system with audit trails.
- Test every incoming component. No exceptions.
- Don’t wait for an inspection. Do your own internal audits monthly.
It takes 18 to 24 months from ground-breaking to first commercial batch. Rush it, and you’ll fail.
Final Thought: It’s Not About Cost. It’s About Trust.
Generic drugs save the U.S. healthcare system over $300 billion a year. But that savings only works if people trust them. If patients start doubting whether their $5 pill is safe, the whole system crumbles.CGMP isn’t a burden. It’s the foundation. It’s what lets a nurse hand a diabetic their insulin without wondering if it’s been contaminated. It’s what lets a parent give their child an antibiotic without fear.
The FDA doesn’t enforce CGMP to punish companies. They enforce it because someone’s life depends on it.
Are CGMP requirements different for generic drugs compared to brand-name drugs?
No. The FDA requires identical CGMP standards for both generic and brand-name drugs. A generic pill must be manufactured under the same conditions, with the same controls, testing, and documentation as the original. This ensures pharmaceutical equivalence - meaning the generic works the same way in the body. The law doesn’t allow lower standards for generics.
What happens if a generic drug factory fails an FDA inspection?
The FDA issues a Warning Letter, which becomes public. If the issues aren’t fixed within the deadline, the agency can block imports, issue an import alert, or even seek a court order to shut down operations. In severe cases, the company may face civil penalties of up to $1 million per violation. Repeated failures can lead to consent decrees - legally binding court orders requiring full system overhaul under federal supervision.
How often does the FDA inspect generic drug manufacturers?
Domestic facilities are inspected about 1.3 times per year on average. Foreign facilities are inspected less frequently - roughly half as often. However, the FDA’s 2023-2027 plan includes a 25% increase in resources for foreign inspections, meaning this gap is expected to narrow in the coming years. Inspections are risk-based, so facilities with past violations or high-risk products get inspected more often.
What are the most common CGMP violations in generic drug manufacturing?
In 2022, the top two violations were related to production and process controls (§ 211.100) and laboratory controls (§ 211.160), accounting for 41% of all citations. Other frequent issues include data integrity failures (especially in electronic records under Part 11), inadequate cleaning validation, and failure to test incoming components. Foreign facilities are disproportionately cited for data integrity problems.
Can a generic drug be approved without CGMP compliance?
No. CGMP compliance is mandatory for every Abbreviated New Drug Application (ANDA) submitted to the FDA. The agency reviews manufacturing practices as part of the approval process. If the facility isn’t compliant, the application is denied - even if the drug’s chemistry and effectiveness are perfect. You cannot legally sell a generic drug in the U.S. without passing CGMP inspection.
Is electronic recordkeeping required for CGMP compliance?
Yes. While paper records are still technically allowed, the FDA strongly expects electronic systems with audit trails under 21 CFR Part 11. Most large manufacturers use electronic quality management systems (eQMS). Paper records are harder to protect from tampering and are more difficult to audit. In practice, companies using paper systems face higher inspection risks and are more likely to receive citations for data integrity issues.


Kathy Scaman
Just saw my pharmacist hand me a generic for my blood pressure med yesterday. Didn’t even blink. That’s because I trust the system. No drama, no guesswork - just science and regulation doing its job.
Anna Lou Chen
Ah, CGMP - the neoliberal sacrament of pharmaceutical orthodoxy. A ritualized performance of compliance that masks the deeper ontological crisis of late-stage capitalism’s commodification of biological life. The FDA doesn’t enforce standards - they enforce epistemic hegemony. Who gets to define 'safe'? Who profits from the myth of equivalence?
Behind every 'identical' pill is a global supply chain of exploited labor, regulatory arbitrage, and the quiet erasure of local pharmacopeias. You call it 'trust.' I call it manufactured consent.
Bryan Fracchia
Anna, I get where you're coming from - the system isn't perfect. But let’s not throw the baby out with the bathwater. The fact that 90% of prescriptions are generics and people are still alive and well? That’s not magic. That’s CGMP working. Real people, real science, real oversight.
Yeah, small manufacturers struggle. Yeah, foreign inspections need more teeth. But the alternative? More metformin recalls. More contaminated antibiotics. More parents wondering if their kid’s medicine is safe. That’s not philosophy. That’s risk.
Lance Long
Let me tell you something - I worked in a small generic lab for five years. We didn’t have a fancy eQMS. We had a printer, three binders, and a team that showed up at 5 a.m. because they knew someone’s life depended on that batch.
Yeah, we were behind on documentation. Yeah, we got nervous before inspections. But we never cut corners on testing. Not once. And when the FDA came? They shook our hands. Said, 'You guys are the reason this system still works.'
Don’t talk about 'epistemic hegemony' when the real heroes are the techs cleaning hoods at midnight. They’re the ones keeping you alive. Not the audits. Not the regulations. Them.
Timothy Davis
Everyone’s acting like CGMP is some sacred text. Let’s be real - 73% of warning letters in 2022 came from foreign facilities, mostly in India and China. The FDA inspects those plants once every 3–5 years. Meanwhile, domestic plants get visited 1.3 times a year. That’s not 'risk-based' - that’s colonial oversight.
And don’t get me started on 'electronic records.' Half the companies using eQMS still have audit trails that can be backdated with a script. The FDA’s Part 11 enforcement? A joke. They’re chasing paper logs while the real fraud happens in SQL databases.
Also, 'three consecutive batches' for validation? That’s a myth. Most companies do one and fudge the rest. The FDA knows. They just don’t have the manpower to catch it. So they pick on the small guys.
fiona vaz
Timothy’s got a point about the inspection gap - it’s real. But I’ve seen small manufacturers turn things around. One in Ohio went from a 48-hour inspection backlog to full compliance in 8 months just by hiring a part-time QA consultant and using open-source eQMS tools.
It’s not about money. It’s about priorities. If you treat compliance like a cost center, you’ll fail. If you treat it like your product’s soul, you’ll survive. And the FDA? They’ll notice. I’ve seen it happen.
Sue Latham
Oh honey, let’s not pretend this is about safety. It’s about branding. The FDA lets big pharma get away with murder - literally - because they’re 'too important to fail.' But a little guy with a $200k budget? One typo in a logbook and he’s banned from the US market.
And don’t even get me started on 'continuous manufacturing.' That’s just Big Pharma’s way of locking out competition. You think a mom-and-pop lab can afford a $12M continuous flow line? Please. It’s not innovation. It’s monopoly maintenance.
John Rose
There’s a deeper truth here: CGMP isn’t about drugs. It’s about trust. In a world where misinformation spreads faster than viruses, the fact that we can hand a $5 pill to someone and know it won’t kill them - that’s extraordinary.
It’s not perfect. It’s not glamorous. But it’s one of the few systems in modern life where accountability is non-negotiable. And that’s rare. We should be grateful, not cynical.
Also - the AI and predictive quality stuff? That’s not sci-fi. It’s happening. I’ve seen prototypes that flag a potential contamination 72 hours before it happens. That’s not just compliance. That’s prevention at scale.
Brittany Fiddes
Oh, please. You Americans think your FDA is some global gold standard? Tell that to the 200 people who died in Pakistan from contaminated cough syrup last year - made by a factory that passed an FDA inspection six months prior.
We in the UK have stricter standards. We audit the entire supply chain. We require batch-level traceability. And we don’t let foreign manufacturers off the hook because they're 'economically important.'
Your system is a patchwork of loopholes and political favors. Don’t mistake bureaucracy for integrity. We don’t need more 'risk-based inspections' - we need real accountability. And maybe, just maybe, stop outsourcing your medicine to countries with zero transparency.