When Your Body Turns Against You, Movement Becomes a Battle
Imagine waking up and your hands feel like they’re wrapped in concrete. Getting out of bed takes five minutes of planning. Cooking dinner? Forget it. Walking to the mailbox leaves you exhausted for hours. This isn’t just fatigue. This is functional impairment - the quiet, crushing reality for millions living with autoimmune diseases like lupus, rheumatoid arthritis, Sjögren’s, and fibromyalgia. It’s not about how bad your blood tests look. It’s about whether you can button your shirt, hold a coffee cup, or stand long enough to wash dishes. And here’s the truth: most doctors don’t talk about this. They treat inflammation. They don’t teach you how to live with it.
But there’s another path. One that doesn’t rely on pills alone. One that helps you take back control, day by day. Rehab and occupational therapy aren’t luxuries. They’re lifelines. And the data proves it: structured programs can improve daily function by 35-42%, according to the Journal of Autoimmunity (2022). That’s not a small win. That’s returning to work, playing with your kids, or finally being able to drive yourself to the pharmacy.
What Exactly Is Functional Impairment in Autoimmunity?
Functional impairment isn’t a single symptom. It’s the sum of many things: joint pain, muscle weakness, brain fog, crushing fatigue, nerve damage, and the side effects of medications. For someone with rheumatoid arthritis, it might mean losing grip strength so you can’t open jars. For someone with lupus, it could be that even standing for five minutes triggers a crash that lasts days. Sjögren’s patients might struggle to type because their fingers are stiff and dry. These aren’t "just bad days." They’re the new normal - until you learn how to fight back.
The problem? Most people wait too long. They push through pain, hoping it’ll get better on its own. By the time they seek help, their muscles have atrophied, their joints have stiffened, and their confidence is gone. Studies show the best outcomes happen when rehab starts within the first 12 months of symptoms. That’s the window where you can still rebuild - before your body adapts to being broken.
Physical Therapy: Rebuilding Strength Without Triggering Flares
Physical therapy (PT) isn’t about lifting heavy weights or running marathons. It’s about smart, precise movement. During a flare, when joints are swollen and hot, PT focuses on gentle isometric exercises - tightening muscles without moving the joint. That’s it. Just 20-30% of your max effort. It keeps your muscles alive without burning you out.
When things calm down, you move to aerobic work: walking, cycling, or swimming at 40-60% of your heart rate reserve. Not 80%. Not "go hard or go home." That’s how people end up in the ER. A 2022 study from the Back to Motion database found PT improved lower-body function 28% better than OT alone - measured by how fast you can stand up from a chair, walk three meters, and sit back down. That’s the Timed Up and Go test. It sounds simple. But if you can’t do it in under 12 seconds, you’re at risk of falling. And that’s not a hypothetical.
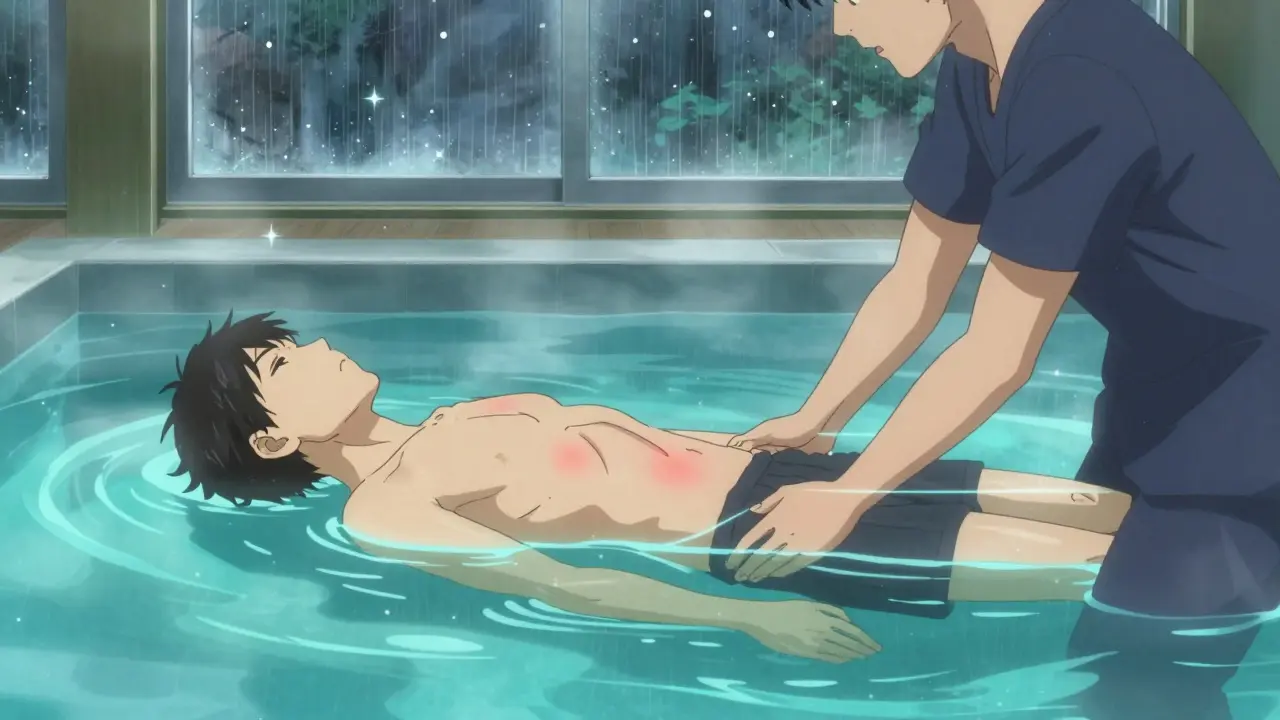
Hydrotherapy is a game-changer. Water at 92-96°F reduces joint pressure and eases pain. One study showed pain scores dropped from 7.2 to 4.1 on the Visual Analog Scale - a 22% better result than land-based exercise. But here’s the catch: 68% of rural rehab centers don’t even have a pool. That’s why home-based programs are rising fast. You don’t need a fancy facility. You need a knowledgeable therapist who knows how to scale intensity.
Occupational Therapy: Reclaiming Your Daily Life
OT doesn’t fix your joints. It fixes your life around them.
Think about the things you do every day: brushing your teeth, opening a medicine bottle, typing an email, carrying groceries. Now imagine doing them with swollen fingers, weak wrists, and zero energy. That’s where occupational therapists step in. They don’t just teach you how to move better. They teach you how to move less - and smarter.
Their secret weapon? The 4 Ps: Prioritize, Plan, Pace, Position.
- Prioritize: What absolutely must get done today? Save the rest.
- Plan: Break tasks into chunks. Don’t clean the whole kitchen. Do one counter at a time.
- Pace: Work for 15-20 minutes. Then rest for 5-10. No exceptions. This stops the boom-bust cycle that leaves you bedridden for days.
- Position: Use your body like a tool. Sit to shave. Use a long-handled sponge. Wear slip-on shoes. Every tiny change adds up.
They also recommend adaptive tools. Voice-activated smart home systems? They’ve been shown to boost independence by 31% for people with hand impairments. Electric jar openers, rocker knives, keyboard stands - these aren’t gadgets. They’re survival tools. And insurance often covers them if your therapist writes a letter.
OT also uses the Canadian Occupational Performance Measure (COPM). It’s not a lab test. It’s a conversation: "What’s something you used to do that you can’t do now?" Then they track progress. A 2-point increase on the 10-point scale? That’s clinically meaningful. That’s you getting back to gardening, reading to your grandkids, or working part-time again.
Why PT and OT Work Better Together
PT gets you moving. OT gets you doing. One isn’t better. They’re different sides of the same coin.
PT improves your leg strength so you can walk to the kitchen. OT teaches you how to use a reacher to grab your coffee mug without bending over. PT helps you climb stairs. OT helps you sit down safely when you get there.
Here’s the data:
| Area of Function | PT Advantage | OT Advantage |
|---|---|---|
| Lower Body Mobility | 28% better improvement | Minimal impact |
| Upper Body Function | Minimal impact | 33% better improvement |
| Activities of Daily Living | 12% improvement | 41% improvement |
| Pain Reduction (Hydrotherapy) | 22% greater reduction | Same benefit |
PT gets you stronger. OT gets you functional. Together? They’re unstoppable.
The Hidden Rules: What No One Tells You
There’s a dark side to rehab. And most patients find out the hard way.
First: Don’t push through pain. That’s not grit. That’s self-sabotage. 37% of patients start high-impact workouts - spinning, CrossFit, running - because they’re told "exercise is medicine." But in autoimmune disease, the wrong exercise can trigger a flare that lasts weeks. One study found those patients had 23% more injuries.
Second: Therapists aren’t always trained. Not every PT or OT knows how to handle lupus or Sjögren’s. Look for someone with the Autoimmune Specialty Certification from the Academy of Pelvic Health Physical Therapy. It’s a 120-hour program. Only 78% pass. That’s your filter.
Third: The boom-bust cycle is real. You have a good day. You do everything you’ve been avoiding. Then you crash for three days. 63% of patients do this. The solution? The 70% rule. Never go beyond 70% of your perceived maximum effort. If you feel like you could do more? Stop. You’re not saving energy for tomorrow. You’re stealing it.
And fourth: Insurance won’t cover enough. Most plans pay for 12-15 sessions a year. You need 24-30. That’s why home programs and telehealth are exploding. Post-pandemic, 68% of patients now use virtual rehab. It’s cheaper. More flexible. And just as effective.
What Success Actually Looks Like
It’s not running a 5K. It’s not lifting 50 pounds.
It’s this:
- u/RheumaWarrior on Reddit: "After 6 months of graded exercise, my HAQ-DI score dropped from 2.1 to 0.8. I went from needing help to get dressed to working part-time again."
- A woman in Ohio who stopped using a cane after learning how to pace her walks with her OT.
- A man in Texas who started using voice commands to control his lights, thermostat, and TV - because his hands couldn’t hold a remote anymore.
Success is the quiet victories. The ability to pick up your grandchild. To cook your own meal. To not cry because you can’t open a pill bottle.
And here’s the most important part: it’s not permanent. Your body changes. Your disease changes. So your rehab plan must change too. That’s why tracking matters. Some patients now use wearables that measure heart rate variability - a sign of how stressed your nervous system is. If your HRV drops, you scale back. No guesswork. Just data.
The Future Is Personalized - and It’s Already Here
Rehab is no longer one-size-fits-all. The NIH launched the Autoimmune Rehabilitation Registry in January 2023 to track 5,000+ patients. Why? To find patterns. To see which exercises work best for which people.
And now, new biomarkers like serum IL-6 levels are being used to adjust exercise intensity. If your inflammation marker spikes, your therapist lowers your workload. No more guessing. Just science.
And then there’s AI. The Lupus Foundation’s "PacePartner" app - in Phase 3 trials - uses data from your smartwatch to predict flares 3-5 days in advance with 82% accuracy. It tells you: "Rest today. Your body is signaling a flare." That’s not science fiction. That’s next year.
But here’s the catch: we’re running out of therapists. By 2026, there will be an 18,000-person shortage. That’s why learning to manage yourself is critical. You don’t need to see a therapist every week. You need to know how to listen to your body - and how to ask for help when you can’t.
Where to Start Today
You don’t need to wait for a referral. You don’t need to be perfect. You just need to begin.
- Find a therapist with autoimmune experience. Ask: "Do you have training in autoimmune rehabilitation?" If they look confused, move on.
- Start with the 4 Ps. Write down your daily tasks. Pick one. Break it into 15-minute chunks. Rest. Repeat.
- Buy a simple heart rate monitor. Track your resting HR and HRV. If it spikes 10-15% above baseline, take it easy.
- Use the 70% rule. Always. Even on good days.
- Ask your doctor for a referral to occupational therapy. If they say "you don’t need it," get a second opinion.
This isn’t about fixing your disease. It’s about fixing your life around it. You don’t have to wait until you’re broken to start rebuilding. Start now - with one small, smart step.






Wendy Lamb
Just wanted to say this post hit home. I’ve been living with RA for 12 years, and OT changed everything for me. The 4 Ps? Lifesaver. I used to try to do everything in one go-now I break it down like a recipe. One counter at a time. One dish at a time. It’s not glamorous, but it’s sustainable.
Also, the insurance thing? So true. My therapist wrote a letter for an electric jar opener. Got approved on the first try. That thing is my MVP.
Amit Jain
As someone from India, I can tell you-rehab access is brutal here. No pools, no trained therapists, no insurance coverage. I learned pacing from YouTube videos and a cheap resistance band. It’s not perfect, but it’s something. Start small. Even 5 minutes of gentle movement counts.
Ed Mackey
Hey, I just want to say I read this whole thing. Took me two days. I had to rest in between. But I’m glad I did. The part about hydrotherapy? I tried it last month. My pain score dropped from 8 to 5. Not magic, but real. And I didn’t even have a pool-just a warm bath and a timer.
Also, typo: "back to motion" database? I think you meant "Back to Motion"-but I get what you meant. No biggie.
Keith Harris
Oh wow. Another one of those "exercise is medicine" posts. Let me guess-you also think stretching your hamstrings will cure lupus? Newsflash: autoimmune diseases aren’t solved by willpower. You’re just repackaging toxic positivity as rehab advice.
And don’t get me started on that "70% rule." Sounds like a corporate wellness hack. What about the people who can’t even get out of bed? You’re not helping. You’re preaching.
Prajwal Manjunath Shanthappa
While I appreciate the earnestness of this piece, I must note-with the precision of a trained epistemologist-that its reliance on anecdotal data, coupled with a statistically underpowered citation from the Journal of Autoimmunity (2022), renders its clinical assertions vulnerable to confirmation bias. Moreover, the uncritical endorsement of wearable HRV trackers as diagnostic tools borders on techno-utopianism. One wonders: if we are to rely on biomarkers, why not deploy machine learning models trained on longitudinal cytokine profiles instead of asking patients to "take it easy"?
And yet-
-the emotional valence of the narrative is undeniably compelling. A rhetorical triumph, if not an empirical one.
Mandy Vodak-Marotta
I’m a 38-year-old mom with Sjögren’s and fibro, and I just want to say-this is the first time I’ve read something that didn’t make me feel like a failure. I used to think I was lazy because I couldn’t clean the house in one day. Turns out, I just needed to stop trying to be Supermom and start being Me. The 4 Ps? I wrote them on a sticky note and put it on my fridge. PACE. PACE. PACE.
I also bought a rocker knife. It’s not sexy. But I made pancakes last week. With my own hands. And I didn’t cry. That’s a win.
Also, if you’re reading this and you’re new to this? You’re not alone. I used to think I was the only one who cried over a pill bottle. Turns out, everyone does. We just don’t talk about it.
Kunal Kaushik
Man, this hit different. I’ve been dealing with lupus for 8 years. I used to think I had to push through. Now I just rest. And sometimes, that’s enough. No guilt. No pressure. Just… breathe.
Also, hydrotherapy. I live in a city with no pools. So I use my bathtub. Hot water. 20 minutes. Then I lie down. That’s my new religion.
Antwonette Robinson
Oh wow. A post that doesn’t just say "exercise is medicine" and call it a day? Groundbreaking. Next you’ll tell us water is wet and gravity exists.
But seriously-how many people are going to read this and think, "Oh, I just need to try harder?" Meanwhile, the real issue is that the healthcare system doesn’t fund this stuff. Not the 70% rule. Not the 4 Ps. Not even a damn electric jar opener. You’re giving people a hammer and calling it a solution while the house burns down.
Jesse Naidoo
Wait-so you’re telling me I’m supposed to stop pushing through pain? What, like, ever? I’ve been told for years that pain is just a sign I’m getting stronger. Now you’re saying that’s wrong? I feel like I’ve been lied to my whole life.
Also, I tried OT. The therapist said I needed a reacher. I laughed. Then I cried. Then I bought one. And now I can grab my phone off the floor without asking my partner. That’s… kind of a big deal.
Daz Leonheart
I’ve been doing this for years. PT and OT. Graded exposure. Pacing. The 70% rule. I didn’t believe it at first. Thought it was too soft. But after 18 months? I’m working part-time. I cook dinner. I play with my dog. I don’t need help anymore.
It’s not fast. It’s not flashy. But it works. If you’re reading this and you’re stuck? Start with one thing. One small thing. And do it slow.
Roshan Gudhe
There’s a quiet dignity in learning how to live with a body that betrays you. It’s not about curing. It’s about adapting. About becoming intimate with your limits-not as a defeat, but as a form of wisdom.
I used to think strength meant pushing harder. Now I know: true strength is knowing when to stop. When to rest. When to ask for help. When to let go of the idea that you have to earn your right to exist.
And maybe that’s the real therapy.
Rachel Kipps
I appreciate the thoroughness of this article. The data points are well-sourced, and the emphasis on functional outcomes over laboratory markers is refreshing. That said, I do wonder if the reliance on telehealth and home programs may inadvertently widen disparities for those without reliable internet, stable housing, or caregiver support.
Perhaps future iterations could include a section on navigating systemic barriers-especially for marginalized communities.
Harriot Rockey
This gave me chills. I’m a nurse who’s lived with lupus for 15 years. I’ve seen so many patients give up because no one told them rehab could help. I wish I’d known this 10 years ago.
One thing I’d add: don’t wait for a referral. Call your local rehab center yourself. Ask for the therapist who does autoimmune cases. If they don’t have one, ask if they’ll train someone. Demand it.
You deserve to live. Not just survive. Live.
Alex LaVey
For anyone feeling overwhelmed: you’re not broken. You’re adapting. And that’s brave.
I used to think I had to be "productive" to matter. Now I know: resting is revolutionary. Pacing isn’t laziness-it’s strategy. And asking for help? That’s courage.
You’re not alone. We’re here.
Nathan King
While the intent of this article is commendable, its rhetorical structure betrays a fundamental epistemological flaw: it conflates anecdotal efficacy with clinical generalizability. The reliance on self-reported outcomes-particularly from Reddit users-lacks the methodological rigor required for evidence-based practice. Furthermore, the uncritical adoption of proprietary tools like the "PacePartner" app, still in Phase 3 trials, constitutes premature scientism.
One must ask: if this model is so effective, why is it not universally integrated into national healthcare systems?