Imagine you’re having a panic attack. Your heart is racing, you can’t breathe, and the world feels like it’s collapsing. You take a pill - and within minutes, the storm inside you calms down. That’s what benzodiazepines do. They’re powerful, fast-acting drugs that can save someone from a crushing moment of fear. But for many, what starts as relief turns into a trap. The same pills that bring peace can steal your independence, your memory, and sometimes, your life.
How Benzodiazepines Work
Benzodiazepines don’t just make you feel calm - they change how your brain works. They boost a natural chemical called GABA, which acts like a brake pedal for your nervous system. When GABA fires, it tells overactive neurons to slow down. That’s why these drugs work so fast: they silence the noise in your brain that causes anxiety, seizures, and muscle spasms.
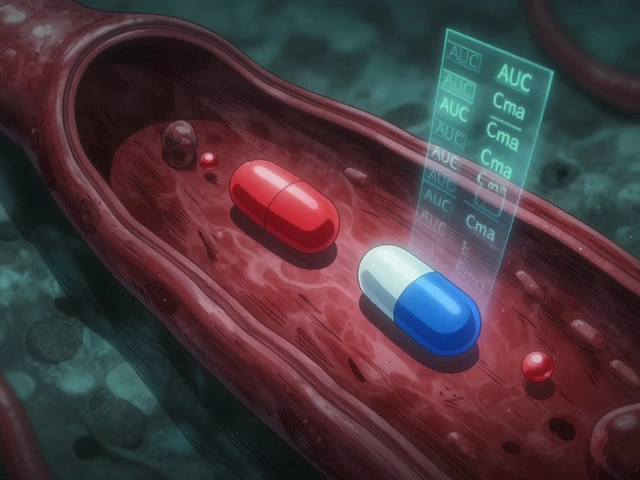
There are over a dozen types, but they all follow the same rule: the shorter the half-life, the quicker they kick in - and the harder they are to quit. Triazolam and alprazolam wear off in hours. Diazepam and clonazepam stick around for days. That’s why doctors pick one over another. Short-acting ones like lorazepam are used for panic attacks or before surgery. Long-acting ones like diazepam help with alcohol withdrawal or chronic muscle spasms.
These aren’t magic bullets. They don’t fix the root cause of anxiety. They just mute the symptoms. And that’s where the danger begins.
The Real Benefits - When Used Right
Benzodiazepines are lifesavers in emergencies. In a hospital, midazolam stops seizures that won’t quit. In the ER, diazepam calms violent muscle contractions. For someone with severe insomnia after a trauma, a short course of temazepam can restore sleep when nothing else works.
For acute anxiety - like fear of flying, a panic attack before a job interview, or grief after a loss - they offer relief no other drug can match. While antidepressants like sertraline take weeks to work, a single dose of alprazolam can bring calm in under an hour. That’s why they’re still used: because sometimes, waiting isn’t an option.
Studies show 60-80% of people get immediate relief from panic attacks with these drugs. On Reddit’s r/Anxiety forum, 68% of users said benzos gave them their first real sense of control. For some, that’s enough to get through a crisis.
But here’s the catch: that relief is temporary. After just two to four weeks, your brain adapts. The same dose stops working. You need more. And that’s when dependence starts.
The Hidden Risks - Even at Prescribed Doses
Most people think if a doctor prescribed it, it’s safe. That’s not true.
Physical dependence develops in 30-50% of people who take benzodiazepines for more than four weeks - even if they follow the prescription exactly. Your body starts to need the drug just to feel normal. Stop it suddenly, and your brain goes into overdrive. You get rebound anxiety worse than before. Tremors. Insomnia. Hallucinations. Seizures.
One in five users report memory gaps. You might forget conversations, meals, or even driving to work. That’s anterograde amnesia - not a side effect, it’s a direct result of how these drugs work. They block the brain from forming new memories.
Older adults are especially vulnerable. The American Geriatrics Society says benzos increase fall risk by 50% in people over 65. They also raise dementia risk by 32% with long-term use. That’s why doctors are now told to avoid them in seniors entirely.
And then there’s the emotional toll. Many users describe feeling numb. Not peaceful - just empty. Like they’re watching life through fogged glass. That’s not healing. That’s suppression.
Dependence Isn’t Addiction - But It’s Just as Dangerous
Dependence isn’t the same as addiction. Addiction means you’re using drugs to get high, chasing pleasure, ignoring consequences. Dependence means your body can’t function without the drug - even if you don’t want it.
People on long-term benzos often feel trapped. They know they should quit. But the thought of withdrawal terrifies them. One woman in a UK support group told me she’d been on diazepam for 12 years. She didn’t like it. She hated the fog. But she couldn’t sleep without it. And when she tried to stop, she had panic attacks so bad she ended up in A&E.
Withdrawal isn’t just uncomfortable. It can be deadly. Seizures, delirium, psychosis - these aren’t rare. They happen when people quit cold turkey. That’s why tapering is non-negotiable. The Ashton Manual, the gold standard for quitting benzos, says most people need 3-6 months to safely reduce their dose. Some need over a year.
And here’s the worst part: most doctors don’t know how to help. A 2021 study found that 61% of problematic cases came from patients who were never given a plan to stop. They were just handed a script and told to take it as needed. That’s not treatment. That’s negligence.
Why Alternatives Are Better - and What Works Instead
Antidepressants like SSRIs don’t work overnight. But they work for years. They fix the chemistry behind anxiety, not just mask it. They don’t cause memory loss. They don’t lead to dependence. And they’re far safer for long-term use.
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the most effective treatment for chronic sleep problems - and it has zero risk of addiction. Studies show it works better than sleeping pills after six months. For anxiety, CBT reduces symptoms as well as benzos - without the crash when you stop.
And here’s the breakthrough: combining low-dose benzos with CBT cuts dependence risk by 58%. That’s the future. Not lifelong pills. Not abrupt stops. A bridge - short, supervised, and intentional.
UK’s NICE guidelines now say: don’t start benzodiazepines for anxiety. Ever. Not even for a week. That’s because the risk outweighs the benefit. In the US, Kaiser Permanente cut long-term prescriptions by 37% just by adding alerts in their electronic records. They didn’t ban them. They just made doctors think twice.

How to Use Them Safely - If You Must
If your doctor says you need a benzo, ask these questions:
- What’s the exact reason? Is this for a crisis, or for something I’ll have for months?
- How long am I allowed to take it? Write it down.
- What’s the plan to stop? Don’t let them say ‘we’ll see.’ Get a taper schedule.
- Are there alternatives? Can we try CBT or an SSRI first?
If you’re already on them, don’t quit cold turkey. That’s how people end up in the hospital. Talk to a specialist. Use the Ashton Manual as a guide. Reduce by 5-10% every 1-2 weeks. Keep a journal. Track your sleep, your mood, your tremors.
And if your doctor won’t help you taper - find another one. There are clinics in Bristol, London, and Manchester that specialize in benzo withdrawal. You don’t have to suffer alone.
The Bottom Line
Benzodiazepines are tools - not solutions. They’re for emergencies, not everyday life. They’re for days, not years. They’re for people who are truly in crisis - not those who just feel a little stressed.
They saved lives in the 1960s. They still save lives today - in ERs, in ICUs, during seizures. But for anxiety? For sleep? For daily stress? They’re outdated. Dangerous. And increasingly, unnecessary.
The real healing comes from therapy, routine, movement, and time. Not a pill that silences your mind - but doesn’t fix what’s broken underneath.
If you’re on benzos and want out - you’re not weak. You’re brave. And you’re not alone.
Can you get addicted to benzodiazepines if you take them as prescribed?
Yes. Physical dependence can develop in 30-50% of people who take benzodiazepines for more than four weeks - even if they follow their doctor’s instructions exactly. Dependence means your body adapts to the drug and needs it to function normally. This is not the same as addiction, which involves compulsive use for pleasure, but it’s still dangerous. Stopping suddenly can cause seizures, severe anxiety, and hallucinations. Always work with a doctor to taper off safely.
How long is it safe to take benzodiazepines?
Most medical guidelines, including those from the American Psychiatric Association and the UK’s NICE, recommend benzodiazepines for no longer than 2-4 weeks. After that, tolerance builds, meaning the drug stops working as well. The risk of dependence rises sharply after four weeks. For insomnia, even short-term use beyond two weeks increases the chance of rebound sleep problems. Long-term use is no longer considered medically appropriate for anxiety or sleep disorders.
What are the most common side effects of benzodiazepines?
Common side effects include drowsiness, dizziness, confusion, impaired coordination, memory problems (especially anterograde amnesia - forgetting events while on the drug), fatigue, and slowed reaction times. Some people experience increased anxiety, tremors, or gastrointestinal issues. In older adults, these drugs significantly raise the risk of falls and hip fractures. Long-term use is linked to a 32% higher risk of dementia.
Can benzodiazepines be used for chronic anxiety?
No. Major health organizations, including the NHS, NICE, and the American Psychiatric Association, no longer recommend benzodiazepines for chronic anxiety. They are ineffective over time due to tolerance and carry high risks of dependence, cognitive decline, and withdrawal. SSRIs, SNRIs, and cognitive behavioral therapy (CBT) are safer and more effective for long-term management. Benzodiazepines should only be used briefly during acute crises or as a temporary bridge while starting other treatments.
What’s the safest way to stop taking benzodiazepines?
The safest way is a slow, medically supervised taper. The Ashton Manual is the gold standard - it recommends reducing your dose by 5-10% every 1-2 weeks. For people on long-term use, this can take 3-6 months or longer. Abruptly stopping can cause seizures, psychosis, or life-threatening withdrawal. Never quit on your own. Work with a doctor who understands benzo withdrawal. Some clinics specialize in this. Support groups and therapy can also help manage symptoms during tapering.
Are there safer alternatives to benzodiazepines for anxiety and sleep?
Yes. For anxiety, SSRIs (like sertraline) and SNRIs (like venlafaxine) are first-line treatments. They take 4-6 weeks to work but have no addiction risk. For insomnia, CBT-I (Cognitive Behavioral Therapy for Insomnia) is more effective long-term than sleeping pills. For acute panic, breathing techniques, mindfulness, and grounding exercises can be powerful. In emergencies, a single dose of a benzo may be appropriate - but only as a bridge, not a solution.
If you’re considering stopping benzodiazepines, start by talking to your doctor - or find a specialist in withdrawal management. You don’t have to live with the fog. There’s a way out.




Virginia Seitz
I was on lorazepam for 3 months after my mom died. It saved me. Now I’m off and I cry more… but I feel real again. 🙏
Peter Ronai
This is pure fear-mongering. People have been using benzos since the 60s and we’re still here. The real crisis is that doctors are too scared to prescribe anything anymore. You want to be numb? Go meditate. Or join a cult.
Michael Whitaker
I must respectfully submit that the conflation of dependence with addiction is not only semantically imprecise, but clinically misleading. The pharmacological profile of benzodiazepines necessitates a nuanced understanding of neuroadaptation-not moral panic. Furthermore, the Ashton Manual, while venerable, lacks randomized controlled trial validation.
Naomi Lopez
The fact that you’re even asking if you can get addicted while taking them 'as prescribed' is the problem. Prescribed doesn’t mean safe. It means someone with a 7-minute consult thought you’d be fine.
Salome Perez
I’m a psychiatric nurse and I’ve seen too many patients trapped in the fog. One woman told me she hadn’t cooked her own dinner in 8 years because she was too dazed to remember how. Benzos aren’t evil-but using them like toothpaste? That’s the tragedy. CBT-I changed my life. So did yoga. And yes, it took time. But I woke up.
Kent Peterson
I’ve been on clonazepam since 2011. I’ve got a PhD. I pay taxes. I vote. I don’t need some ‘NICE guideline’ telling me what my brain needs. You people are just scared of real medicine. You’d rather take kale smoothies and call it ‘therapy.’
Linda Caldwell
You’re not broken. You’re not weak. You’re just tired. And healing isn’t a race. One step. One breath. One day at a time. You’ve got this.
Anna Giakoumakatou
Ah yes, the classic ‘CBT is better’ sermon. Because nothing says ‘I’ve conquered my demons’ like paying $200/hour to talk about your childhood while sipping oat milk lattes. Meanwhile, my diazepam lets me hug my kids without crying. That’s not suppression. That’s survival.
Donna Packard
I’ve been tapering for 11 months. Some days are hell. But today? I remembered my daughter’s laugh. And I didn’t need a pill for that.
Sam Clark
The clinical evidence supporting short-term, supervised benzodiazepine use in acute anxiety disorders remains robust. However, the absence of a structured discontinuation protocol constitutes a significant therapeutic gap. I strongly encourage patients to engage with withdrawal-specialized providers and to document symptom progression throughout tapering.
Chris Van Horn
THIS IS WHY AMERICA IS FALLING APART. YOU LET A FEW DOCTORS AND A HANDFUL OF PSYCHOLOGISTS TELL YOU HOW TO LIVE YOUR LIFE? I TOOK BENZOS FOR 20 YEARS AND I’M STILL ALIVE. I’M STILL WORKING. I’M STILL A FATHER. YOU WANT TO TAKE MY PILLS? COME AND GET THEM. #AMERICA
amanda s
I’m a veteran. I was given Xanax after my third deployment. I’ve been on it since 2015. I don’t care what your ‘guidelines’ say. This pill keeps me from shooting myself. So if you’re gonna take it away, at least give me something better. Or shut up.
Steven Lavoie
I used to be the guy who said ‘just meditate.’ Then my sister overdosed trying to quit cold turkey. Now I help people taper. It’s slow. It’s ugly. But it’s possible. And you don’t have to do it alone. DM me if you need a listening ear.